Chapter 5: Micronutrients
By Mary Marian, DCN, RDN, FAND, FASPEN; Bahar Bakhshi, MS
Student contributor: Ame Proietti
Introduction
Micronutrients include vitamins, minerals, and trace elements that are required in small amounts for normal growth and development and to support several bodily functions. Micronutrients perform a range of functions, such as supporting the synthesis of enzymes, hormones, and other biological compounds needed for growth and optimal function, including the metabolism of the macronutrients discussed in chapter 4.
Micronutrient deficiencies cause visible and dangerous health conditions. They also can contribute to less clinically notable reductions in energy level, mental acuity, and overall functional capacity, as well as an increased risk for other diseases and health conditions. Deficiencies are generally preventable through the consumption of a variety of foods, although certain populations (e.g., pregnant or lactating individuals, elderly adults, young children, individuals with food insecurity) might have difficulty correcting deficiencies with food alone.
Culinary medicine seeks to prevent or address micronutrient deficiencies through nutrition education, including increasing one’s knowledge of the nutrients in various foods, food fortification, and supplementation, and the development of culinary skills that support the preparation of diverse foods.
Micronutrients
Micronutrients—including vitamins, minerals, and trace elements—are inorganic compounds essential for health and wellness. The body is unable to synthesis or store many of these micronutrients, so to meet the body’s daily needs, these compounds must be obtained from one’s diet (through consumption of food and/or dietary supplements) and/or specialized nutrition support (enteral or parenteral nutrition).
Well-planned diets can ensure that healthy individuals consume adequate amounts of micronutrients. Various eating plans, such as the Mediterranean or the Dietary Approaches to Stop Hypertension (DASH) diets, are associated with preventing or managing various health conditions, including cardiovascular disease, hypertension, type 2 diabetes, and certain cancers. Fruits, vegetables, whole grains, nuts, and seeds form the foundation of these eating patterns.
These various foods provide micronutrients that play a key role in health and wellness. The principles of culinary medicine are grounded in the mantra “where health meets foods.” Micronutrient availability and, ultimately, their use by the body are influenced by many factors, including where food is grown and how it is transported, processed, and prepared. But it also is affected by one’s medical history and current health status.
Previous chapters have reviewed food preparation and cooking methods that promote the preparation of high-quality whole foods and meals. Furthermore, well-planned diets can ensure that healthy individuals consume adequate amounts of micronutrients. This chapter will review the key functions and recommended intake levels of micronutrients, factors that influence micronutrient availability and that may promote deficiency, food sources, and biomarkers for assessing status and need for possible supplementation. Also described are the use of popular diets by consumers and their impact on micronutrient provision.
Understanding the relationship between food and micronutrient provision is an essential component that aligns with the application of culinary medicine principles to promote disease prevention and management through the consumption and enjoyment of healthy, tasty food.
Micronutrient Needs
The Dietary Reference Intakes (DRIs)—created by the Food and Nutrition Board of the National Academies of Sciences, Engineering, and Medicine and promoted in established guidelines—have set reference micronutrient intake values for all generally healthy Americans.1 These values are based on age and sex. For women, values vary based on pregnancy and lactation. However, individual needs may be lower or higher than these reference values based on health status; therefore, it is important to assess one’s health status before determining interventions.
These standards are used in the design of food labels, for assessing an individual’s adequacy of nutrient dietary intake, and for planning diets. Knowing what the daily intake goals are is essential to know whether dietary intake is sufficient and if supplementation is needed to meet nutrient needs to promote optimal health and wellness.
The DRIs provide a set of recommended values used to assess adequacy of nutrient intake.1-3 Included in this set of guidelines are:
- Adequate Intake (AI)
- Estimated Average Requirement (EAR)
- Recommended Dietary Allowance (RDA)
- Tolerable Upper Intake Level (UL)
A digital daily calculator is available to assist health-care professionals in evaluating the adequacy of intake.2 This is useful to provide recommendations for achieving optimal micronutrient status.
The RDA values reflect the level of a specific nutrient that 98% of a generally healthy population needs.1 This is because RDAs are set 2 standard deviations above the EAR values, which establishes a margin of safety for intake.
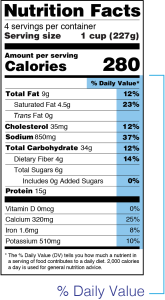
Food labels can provide valuable information to help consumers determine what micronutrients (and how much of them) are in a product. However, food labels can be confusing because they use the Daily Value (DV) or percent DV (%DV) instead of the DRIs.3 Although the DV is similar to the DRIs, the DV is not differentiated by age and sex, like the RDAs. Daily Values have been established by the US Food and Drug Administration (FDA), and before 2016, there was only 1 DV for each of the micronutrients.3
For example, the %DV labels for iron is 18 milligrams (mg). However, the RDA for adult men is 8 mg per day; for women, 18 mg per day reflects the RDA for premenopausal women, and the RDA decreases to 8 mg per day for postmenopausal women. This difference in values can be confusing for consumers when trying to determine which foods will help meet their nutritional needs.
Labels are also only required to reflect the DVs for calcium, vitamin D, potassium, and iron.3 The other micronutrients are not required to be listed, but they can be, at the discretion of the manufacturer.
The DVs reflect the percentage of a nutrient a product will provide as it relates to the “highest” RDA based on age and sex (see Figure 5.1). For example, related to iron, the %DV listed on a food label correlates with the RDA for premenopausal women (18 mg), which is the highest of the various RDAs for age and sex.
Vitamins
Vitamins can be obtained from a variety of different foods and are classified as either water soluble or fat soluble. Various mechanisms in the small intestine are responsible for the absorption of vitamins. A major difference between the 2 types of vitamins is that fat-soluble vitamins are absorbed with fat. The following discussion describes the role each vitamin plays in promoting health and wellness, in addition to reviewing: recommended intake levels, food sources, recommended biomarkers for assessing status, signs of deficiencies, and populations at risk.
Water-Soluble Vitamins
There are 9 water-soluble vitamins. They, in addition to other vitamins, play a role in metabolism, primarily as cofactors or coenzymes necessary in the formation and storage of energy (see Table 5.1). Although only needed in small quantities by the body, water-soluble vitamins cannot be synthesized or stored by the body. Thus, they are required daily to meet one’s needs; in some cases, deficiencies that increase risk for illness and death can develop very quickly.
Table 5.1. Water-Soluble Vitamin Functions5-13
|
B vitamins |
|
|---|---|
| Thiamine (B1) | Required in energy transformation, synthesis of pentoses and reduced nicotinamide adenine dinucleotide phosphate (NADPH), and nerve conduction. Plays a major role in carbohydrate metabolism and serves as a magnesium-coordinated coenzyme for oxidative decarboxylation of α-ketoacids (e.g., pyruvate). Deficiencies can arise with alcohol abuse, diuretic use, and malabsorption. |
| Riboflavin (B2) | Primary function is as a component of the flavin mononucleotide and flavin adenine dinucleotide as an electron transport intermediary for oxidation-reduction reactions. Also has antioxidant properties. Deficiency is rare. |
| Niacin (B3) |
Nicotinamide portion of nicotinamide adenine dinucleotide and nicotinamide adenine dinucleotide phosphate serves as a hydrogen donor or an electron acceptor for more than 200 enzymes involved in intermediary metabolism of amino acids, carbohydrates, and fatty acids. NADPH is required for activation of folate. Pellagra is the disease caused by niacin deficiency, which is rare in developed nations. Look for the 3 Ds: dermatitis, diarrhea, and dementia. Deficiencies may occur with malnutrition and malabsorption. |
| Vitamin B6 (3 forms: pyridoxine, pyridoxal, and pyridoxamine) |
Coenzyme forms participate in more than 100 enzymatic reactions. Facilitates transamination and deamination. Important for cognitive development. Also assists with decreasing homocysteine levels. Pyridoxine is converted to the active coenzyme pyridoxal phosphate and coenzyme pyridoxamine to pyridoxamine phosphate. |
| Vitamin B12 | Needed for the conversion of homocysteine to methionine. Elevated homocysteine levels have been linked with increased risk for cardiovascular disease, cerebral vascular accident, dementia, Alzheimer’s disease, and osteoporosis. When B12 is lacking, folate is “trapped” in its inactive form. B12 is also needed for erythrocyte synthesis. Deficiencies may occur with malabsorption, inadequate intake, and use of certain medications. |
| Other vitamins | |
| Folic acid |
Primary function is as a coenzyme in the transfer of single-carbon fragments from 1 compound to another for amino acid metabolism and nucleic acid synthesis. There is increased demand for folate during pregnancy, due to increased demand for DNA synthesis for embryonic development. Folate deficiency causes the misincorporation of uracil in place of thymine, leading to DNA fragility and strand breakage that cause neural tube defects (NTDs) during fetal development. Since the FDA mandated folate fortification of cereal and grain products in 1998, incidence of NTDs has declined. |
| Vitamin C | Antioxidant; synthesis of collagen, carnitine, and neurotransmitters; enhances intestinal absorption of nonheme iron, and immune-mediated and antibacterial functions of white blood cells. Deficiency can be caused by inadequate intake and malabsorption. |
| Pantothenic acid (PA) | As a component of coenzyme A, PA is involved in energy production from fat, carbohydrates, and ketogenic amino acids. Also required for the synthesis of bile salts, cholesterol, steroid hormones, and fatty acids. Deficiency is rare. |
| Biotin | Necessary for genetic expression of more than 2,000 enzymes; also needed as a cofactor for several carboxylase enzymes required for metabolic pathways, such as gluconeogenesis and fatty acid synthesis. Deficiency is rare because biotin can be synthesized by colonic microflora. |
Table 5.2 illustrates the daily recommendations for water-soluble vitamin intake for adults based on sex and ULs. Rich food sources for each vitamin, in addition to recommended biomarkers for assessing micronutrient status, are also listed.
Table 5.2. Water-Soluble Vitamin Recommendations5-13
| Water-soluble vitamin | RDA/AI: adult men | RDA/AI: adult women | Tolerable Upper Intake Level | Rich food sources | Recommended biomarkers for assessing status |
|---|---|---|---|---|---|
| Thiamine | 1.2 mg/d | 1.1 mg/d | ND | Pork, fortified/enriched foods, sunflower seeds, wheat germ | Whole blood or erythrocyte thiamine diphosphate |
| Riboflavin | 1.3 mg/d | 1.1 mg/d | ND | Fortified/enriched foods, dairy | Erythrocyte glutathione reductase |
| Niacin | 16 mg/d | 14 mg/d | 35 mg/d | Poultry, fish, beef, fortified/enriched foods | Urinary N1-methyl-nicotinamide and N1-methyl-2-pyridone-5-carboxamide |
| Pyridoxine (vitamin B6) | 1.3 mg/d | 1.3 mg/d | 100 mg/d | Fortified/enriched foods, garbanzo beans, salmon | Plasma pyridoxal 5′-phosphate |
|
Folic acid |
400 mcg/d | 400 mcg/d | 1,000 mcg/d | Spinach, fortified foods such as cereals and pastas, lentils, legumes, asparagus | Red blood cell folate |
| Vitamin B12 | 2.4 mcg/d | 2.4 mcg/d | ND | Liver, clams, oysters, fortified cereals, cottage cheese, animal products, fortified vegan foods | Methylmalonic acid levels; serum B12 levels; always assess folate status simultaneously |
| Pantothenic acid | 5 mg/d | 5 mg/d | ND | Beef liver, fortified/enriched foods, shitake mushrooms, sunflower seeds | Whole-blood pantothenic acid |
| Biotin | 30 mcg/d | 30 mcg/d | ND | Egg yolks, nuts, legumes | Urinary 3-hydroxyisovaleric acid |
| Vitamin C |
90 mg/d Smokers: 125 mg/d |
75 mg/d Smokers: 115 mg/d |
2,000 mg/d | Citrus, tomatoes, strawberries, peppers | Plasma vitamin C or leukocyte vitamin C |
| Abbreviations: AI = Adequate Intake; d = day; ND = not determined; mcg = microgram; mg = milligram; RDA = Recommended Daily Allowance. | |||||
Given the body’s inability to store the water-soluble vitamins, deficiencies can develop quickly for a myriad of reasons. Table 5.3 reflects the populations at risk for deficiencies.
The small intestine is responsible for the digestion and absorption of most micronutrients. Therefore, any conditions that impair these functions or resections of the gastrointestinal tract can lead to the development of deficiencies. Chronic systematic inflammation also adversely affects metabolism of several water-soluble vitamins, including pyridoxine, folate, and vitamin B12.9,10 Furthermore, prescribed medications, disordered eating styles, alcohol abuse, and health status can lead to alterations in micronutrient status.
Table 5.3. Water-Soluble Vitamin Clinical Relevance Summary5-13
| Vitamin | Signs and symptoms | Conditions that increase risk | Repletion dose | Other notable details |
|---|---|---|---|---|
| Thiamine (B1) | Ocular abnormalities, nystagmus, gait ataxia, and mental status changes (Wernicke encephalopathy; wet or dry beriberi) | Bariatric surgery, malabsorptive disorders, protracted vomiting, alcohol abuse, malnutrition with or without hyper-metabolism, diuretics, dialysis |
Varies: Suspected Wernicke encephalopathy: 100-200 mg/d IV or 3 times/d IM for 3-5 days; 100 mg/d, 3 times/d for 1-2 weeks thereafter Confirmed: 200-500 mg 3 times/d for 5-7 days |
Deficiency promoted by intake of glucose without adequate thiamine. Deficiency can develop in 9-18 days. Associated with refeeding syndrome. Adequate Mg2+ needed for activation. DNI: diuretics increase urinary excretion |
| Riboflavin (B2) | Angular stomatitis, cheilosis, glossitis, preeclampsia in pregnancy | Malabsorptive disorders, alcohol abuse, malnutrition, pregnancy, vegans | 5-30 mg/d in divided doses | Deficiency is very rare. High doses can be used to treat migraines (400 mg/d). |
| Niacin (B3) | Thickening and rash on sun-exposed skin, dementia, diarrhea, fatigue | Malabsorptive disorders, alcohol abuse, malnutrition | 300 mg/d in divided doses for 3-4 weeks | High doses can be used to treat dyslipidemia under medical supervision (500 mg/d to 2,000 mg/d). |
| Pyridoxine (B6) | Peripheral neuropathy, hyperhomo-cysteinemia, confusion, dermatitis, glossitis, microcytic anemia | Malabsorptive disorders, alcohol abuse, dialysis, eating disorders | 50-100 mg/d |
High doses can be used to treat nausea and vomiting in pregnancy (10-25 mg/d 3-4 times/d). Can be used to treat neuropathy (1-6 g/d for 12-24 months) but also may not be beneficial. High doses can be neurotoxic and increase the risk for hip fractures in postmenopausal women. DNIs: isoniazid |
| Folic acid (B9) | Macrocytic anemia, cheilosis, CVD, dementia, hyperhomo-cysteinemia | Alcohol abuse, malabsorptive disorders, prenatal, pregnancy, dialysis |
1-5 mg/d Check B12 levels |
DNIs: ↓ levels with phenytoin, methotrexate, sulfasalazine, triamterene; ↓ absorption with pancreatic enzymes and metformin |
| Vitamin B12 | Megaloblastic anemia, depression, glossitis, neuropathy, confusion and cognitive decline, hyperhomo-cysteinemia | Malabsorptive disorders, ileostomy, low gastric HCl output, vegans, vegetarians | 100-1,000 mcg IM/month; standard MVM for vegans and others | DNIs: proton-pump inhibitors, over-the-counter contraceptives, metformin ↓ B12 absorption |
| Vitamin C | Scurvy, delayed wound healing, petechiae, corkscrew hairs, bleeding gums; splinter hemorrhages under the nails | Malabsorptive disorders, malnutrition, dialysis | 100 mg 3 times/d |
Vitamin C assists with iron absorption. DNIs; tetracycline, aspirin, and corticosteroids ↑ urinary excretion |
| Pantothenic acid (B5) | Peripheral neuropathy, fatigue | Severely malnourished | Not available | Deficiency is extremely rare. |
| Biotin | Thinning hair, hair loss, periorificial skin rash and fatigue | Severely malnourished | 2.5 mg/d for 15 months | Deficiency is extremely rare. |
| Abbreviations: CVD = cardiovascular disease; d = day; DNI = drug-nutrient interaction; HCl, hydrogen chloride; IM = intramuscular; IV = intravenous; mg = milligram; Mg2+ = magnesium ion; MVM = multivitamin/mineral. | ||||
A comprehensive nutrition assessment—including an evaluation of weight history, biochemical data, past and current health status, medications prescribed, and use of dietary supplements, in addition to a diet history—can determine if individuals have or are at risk for developing micronutrient deficiencies.
In addition, a nutrition-focused physical exam should be completed to observe for signs of any micronutrient deficiencies that may be present. Niacin, riboflavin, pantothenic acid, and biotin deficiencies are rare in the United States, although when they do occur, deficiencies of several other micronutrients also tend to be present. This can be seen with certain medications, malabsorption, and alcohol abuse.
Therapeutic doses of the water-soluble vitamins are often used for treating certain medical conditions. For example, riboflavin in high doses has been used to treat migraines, and therapeutic doses of niacin are often used to treat dyslipidemia by increasing high-density lipoprotein cholesterol and reducing triglycerides and low-density lipoprotein cholesterol levels (Table 5.3).6,7
Fat-Soluble Vitamins
The fat-soluble vitamins include vitamins A, D, E, and K. Each vitamin has unique characteristics that contribute to overall health and wellness. Fat-soluble vitamins have complex absorption because fat must be present in the gastrointestinal tract at the same time as the vitamin for absorption. The fat-soluble vitamins are necessary for immune function, bone health, vision, and blood clotting (see Table 5.4). In contrast to water-soluble vitamins, fat-soluble vitamins can be stored by the body, so deficiencies can take months to become noticeable.
Table 5.4. Summary of the Fat-Soluble Vitamins Form and Function14-17
| Vitamin | Function(s) |
|---|---|
| Vitamin A: subgroup of retinols; 90% of vitamin A is absorbed; 8% in carotinoids; need fat for absorption of all fat-soluble vitamins | Vision, antioxidant, wound healing |
| Vitamin D (active form: calcitriol/D3) |
Primary role is to maintain serum calcium and phosphorus levels needed to support bone mineralization, neuromuscular functions, calcium absorption, and other cellular functions. Pleiotropic effects*: May reduce risk for cardiovascular disease, promote glucose control and optimal neuromuscular function, reduce the risk for some cancers, reduce the risk for falls, and promote optimal immune function |
| Vitamin E: comprises 8 naturally occurring compounds: 4 tocopherols and 4 tocotrienols. α-Tocopherol is the most active form; functions as an antioxidant; γ-tocopherol is the most abundant dietary form | Neuroprotective; may reduce the risk for certain cancers due to antioxidant benefits; may reduce serum cholesterol levels |
| Vitamin K |
Involved in the clotting cascade and promotes bone health; synthesized by microbes in the small bowel and colon; vitamin K negates the effects of warfarin (patient education often needed regarding this) |
|
*A pleiotropic effect, in this context, refers to when a nutrient deficiency can affect multiple body systems. |
|
Table 5.5 lists the daily recommendations for intake for adults based on sex and upper tolerable limits. Rich food sources in addition to recommended biomarkers for assessing micronutrient status are also shown.14-17
Table 5.5. Fat-Soluble Vitamin Recommendations14-17
| Fat-soluble vitamin | RDA/AI: adult men | RDA/AI: adult women | Tolerable Upper Intake Level | Rich food sources | Recommended biomarkers for assessing status |
|---|---|---|---|---|---|
| Vitamin A | 900 mcg/d | 700 mcg/d | 3,000 IU/d | Orange and yellow vegetables and fruits, fish, liver, dairy, eggs | Serum retinol, serum retinol–binding protein |
| Vitamin D | 15 mcg/d |
19-70 years old: 15 mcg/d >70 years old: 20 mcg/d |
100 mcg/d | Orange and yellow vegetables and fruits, fish, liver, dairy, eggs | Serum 25-hydroxyvitamin D |
| Vitamin E | 15 mg/d | 15 mg/d | 1,000 mg/d | Seeds, nuts, vegetable oils, green leafy vegetables | Serum α-tocopherol |
| Vitamin K | 120 mcg/d | 90 mcg/d | ND | Dark leafy greens, broccoli | Serum phylloquinone, prothrombin time |
| Abbreviations: AI = Adequate Intake; d = day; IU = international unit; mcg = microgram; mg = milligram; ND = not determined; RDA = recommended daily allowance. | |||||
Table 5.6 lists common signs and symptoms that may reflect fat-soluble vitamin deficiencies. Other non-nutritional factors can play a role; therefore, it is important for the health-care professional to consider all factors that may be involved and rule out the possibilities, based on clinical status. Table 5.6 also indicates populations at risk and repletion doses to consider when a deficiency has been identified.
Table 5.6. Summary of Clinical Relevance for Fat-Soluble Vitamins14-17
| Vitamin | Signs and symptoms | Conditions that increase risk | Repletion dose | Other notable details |
|---|---|---|---|---|
| Vitamin A | Night blindness, Bitot spots, poor wound healing, follicular hyperkeratosis | Malabsorptive disorders, poor intake, pregnancy, use of corticosteroids | 3,000-15,000 RAE for 10 days |
DNIs; ↓ absorption with orlistat, mineral oil, cholestyramine ↑ intake may ↑ hip fracture risk |
| Vitamin D | Osteomalacia, hypocalcemia, tetany | Malabsorptive disorders, poor intake, liver or renal dysfunction/dialysis, poor sun exposure, obese | 50,000 IU/wk for 8 weeks → 1,000 IU/d | DNIs: phenytoin, orlistat, mineral oil ↓ absorption; corticosteroids ↓ levels |
| Vitamin E | Vision changes, ataxia, hemolytic anemia; deficiency rare | Malabsorptive/GI disorders, intestinal resection, reduced biliary function | 200-2,000 mg/d |
DNIs: orlistat, mineral oil 800 IU/d may improve NAFLD >400 IU/d may ↑ prostate cancer risk |
| Vitamin K | Bruising, prolonged bleeding, ↓ bone density | Malabsorptive disorders | Not available but typically 2.5-10 mg twice weekly to daily |
DNIs: warfarin; INR goal: 2-3; ↓ absorption with orlistat, mineral oil, cholestyramine Warfarin binds to enteral nutrition tubing; provide more rapid warfarin administration |
| Abbreviations: d = day; DNI = drug-nutrient interaction; GI = gastrointestinal; INR = international normalized ratio; IU = international unit; mg = milligram; NAFLD = nonalcoholic fatty liver disease; RAE = retinol activity equivalent; wk = week. | ||||
Minerals
Similar to vitamins, minerals are classified as elements that are required daily from the diet for health and wellness. Minerals are often organized into 3 categories:
- macrominerals (i.e., calcium, chloride, magnesium, phosphorus, potassium, and sodium)
- trace minerals (i.e., copper, chromium, fluoride, iodine, iron, manganese, molybdenum, selenium, and zinc)
- ultra-trace minerals (i.e., arsenic, boron, nickel, silicon, and vanadium)
In contrast to vitamins, the bioavailability of minerals is often poor, which increases the potential for deficiencies.18 Oxalates, phytates, saponins, and tannins—compounds found in plant-based foods—can interfere with the absorption of calcium, iron, magnesium, and zinc, thereby increasing the potential for deficiencies to develop.
Moreover, excess intake of a particular mineral at 1 time may result in decreased absorption. For example, absorption of calcium is best when consumed in doses of less than 500 mg.19 When daily doses are needed in greater amounts, the doses should be divided and consumed throughout the day. Table 5.7 reflects the functions as well as other notable details for a selection of minerals.
Table 5.7. Summary of Select Minerals and Function19-30
| Mineral | Functions | Notes |
|---|---|---|
| Calcium | Bone and teeth structure; cardiac, neurological, and muscle functions; activation of blood-clotting factors. Higher intakes are associated with lower risk for colon cancer but greater risk for prostate cancer. | The most abundant mineral in the body. The medications classified as aromatase inhibitors (e.g., letrozole, anastrozole, Aromasin [a type of hormone therapy]) prescribed for women with a history of estrogen-positive breast cancer and corticosteroids increase bone loss. Ensure adequate calcium and vitamin D intake. |
| Iron | Iron is an essential component of hundreds of enzymes and proteins that are necessary for critical functions, such as the production of hemoglobin and myoglobin, which transport oxygen; energy production; and DNA synthesis. Iron is also an active site for many reduction-oxidation enzymes involved in metabolism. Necessary for growth, neurological development, and synthesis of some hormones. | Absorption: Absorption mechanisms differ for heme iron and nonheme iron. Heme iron is absorbed intact into the enterocyte (i.e., red blood cell) after the globin fraction is removed, then hydrolyzed to ferrous iron by the intestinal cell. In the stomach, nonheme iron is released from food, usually in the ferric form, and then converted to ferrous iron via the action of gastric acid. The ferrous iron then binds to receptors primarily in the duodenum and jejunum for absorption. |
| Magnesium | Essential in the activation of more than 300 enzymatic reactions; required for maintenance of the sodium-potassium-ATPase pump; structural component of bone, neuromuscular transmission, cardiovascular excitability, vasomotor tone, and muscle contraction. | Intake has generally been reported as inadequate for most adults in the United States. |
| Potassium | Most abundant intracellular cation; needed for sodium-potassium pump and cardiac, muscle, and neurological functions | |
| Sodium | Sodium-potassium pump, fluid/electrolyte balance, and blood pressure | Excess intake increases urinary excretion of calcium. |
| Zinc | Needed in more than 200 enzymatic reactions; cellular proliferation and differentiation; wound healing; insulin synthesis; glucose control; immune function. Can decrease by 50% of the normal level during the acute phase response* due to zinc sequestration. Consider checking C-reactive protein levels to assess level of inflammation. | |
| Copper | Serves as a cofactor for various enzymatic pathways (commonly referred to as “cuproenzymes”) for energy production, iron metabolism, neurotransmission, and connective tissue synthesis | |
| Iodine | Critical component of thyroid hormones and necessary for overall growth and development | |
| Manganese | Serves as a cofactor for many enzymatic pathways involved in antioxidant defenses, metabolism, bone and cartilage formation, and wound healing | Although manganese deficiencies are extremely rare in humans, neurotoxicity issues can arise in the face of disorders associated with manganese-overload disorders and overconsumption of manganese through inhalation, drinking water, and total parenteral nutrition. Individuals with chronic liver dysfunction are also at a high risk for manganese toxicity. |
| Selenium | A major constituent for more than 24 selenoproteins that play an essential role in DNA synthesis, thyroid hormone metabolism, reproduction, and antioxidant functions |
Ultra-Trace Minerals
The ultra-trace minerals, although needed in very small amounts by the body, play a critical role in maintaining health and wellness. Table 5.8 reflects the daily recommendations for intake, upper tolerable limit, and biomarkers that can be used to assess the status of several ultra-trace elements. Information regarding rich dietary sources is also included.
Chromium, molybdenum, and fluoride are additional trace elements needed for various physiological functions for health. The functions of chromium are not well understood, but chromium plays a role in insulin sensitivity and glucose control. As such, chromium supplementation has been promoted for glucose regulation despite clinical research results being inconclusive.
Molybdenum functions as a cofactor for sulfite oxidase, xanthine oxidase, and aldehyde oxidase. Deficiencies in molybdenum have not been reported in healthy adults but may be present in individuals with very rare metabolic disorders.
Even though fluoride helps prevent tooth decay, it is not considered an essential mineral, because it is not required for growth and survival. However, dental caries are a nutritional concern because poor oral health can cause malnutrition related to difficulty chewing. Furthermore, dental caries can ultimately lead to edentulism (partial or total loss of permanent teeth), which can also lead to inadequate nutrient intake and malnutrition because individuals may be unable to consume a variety of foods.30
Table 5.8. Summary of Daily Reference Values, Food Sources, and Biomarkers for Some Minerals19-30
| Mineral | RDA/AI: men | RDA/AI: women | Tolerable Upper Intake Level | Rich food sources | Biomarkers for assessing status |
|---|---|---|---|---|---|
| Calcium |
18-70 y.o.: 1,000 mg/d >70 y.o.: 1,200 mg/d |
18-51 y.o.: 1,000 mg/d >51 y.o.: 1,200 mg/d |
18-50 y.o.: 2,500 mg/d >51 y.o.: 2,000 mg/d |
Dairy foods, kale, broccoli, bok choy, fortified foods such as orange juice and cereal | Serum calcium and ionized calcium levels |
| Iron | >19 y.o.: 8 mg/d |
19-50 y.o.: 18 mg/d >51 y.o.: 8 mg/d |
45 mg/d | Beef, fortified foods, oysters, white beans | MCV/MCHC, ferritin, serum iron |
| Magnesium |
19-30 y.o.: 400 mg/d >31 y.o.: 420 mg/d |
19-30 y.o.: 310 mg/d >31 y.o.: 320 mg/d |
350 mg/d* | Pumpkin seeds, chia seeds, almonds, soy milk, beans | Serum magnesium level |
| Potassium | 3,400 mg/d (AI) | 2,600 mg/d (AI) | ND | Bananas, potatoes, dairy products, tomatoes, oranges/orange juice | Serum potassium level |
| Sodium | 1,500-2,300 mg/d (AI) |
1,500 mg/d-2,300 mg/d (AI) |
<2,300 mg/d | Water, processed foods | Serum sodium level |
| Zinc | 11 mg/d | 8 mg/d | 40 mg/d | Seafood, meats, greens, whole grains | Urinary zinc |
| Trace minerals | |||||
| Copper | 900 mcg/d | 900 mcg/d | 2 mg/d | Shellfish, nuts, seeds | Ceruloplasmin |
| Iodine | 150 mcg/d | 150 mcg/d | 1,100 mcg/d | Iodized salt, seaweed, seafood, eggs, fortified/enriched foods | Urinary iodine levels |
| Manganese | 2.3 mg/d | 1.8 mg/d | 200-600 mg/d depending on body weight | Nuts, seafood, tea, whole grains | Whole-blood manganese levels |
| Selenium | 70 mcg/d | 55 mcg/d | 400 mcg/d | Brazil nuts, seafood, organ meats | Plasma or serum selenium levels; hair and nail selenium levels can also be used |
| Abbreviations: AI = adequate intake; d = day; mcg = microgram; MCHC = mean corpuscular hemoglobin concentration; MCV = mean corpuscular volume; mg = milligram; ND = not determined; y.o. = years old. | |||||
| *Denotes that the Tolerable Upper Intake Level (UL) is higher than the Recommended Daily Allowance (RDA) for men because the UL reflects recommendations based on using magnesium supplements versus the RDA, which is based on intake from food, beverages, and supplements. | |||||
Table 5.9 lists common signs and symptoms that may reflect mineral deficiencies. Because non-nutritional factors can also promote these findings, the health-care professional must discern between nutritional and non-nutritional factors that play a role. Table 5.9 also lists conditions that increase risk for depletion and repletion doses to consider when a deficiency has been identified.
Table 5.9. Mineral Clinical Relevance Summary19-30
| Mineral | Signs and symptoms | Conditions that increase risk | Repletion dose | Other notable details |
|---|---|---|---|---|
| Calcium | Hypocalcemia can result due to low vitamin D status, CKD, Mg deficiency, rickets and osteoporosis, hypotension, tetany, muscle cramps, seizures | Lactose intolerant/milk allergy, female athletes, postmenopausal, dialysis, vegan diets, malabsorptive disorders | 1 g calcium chloride/3 g calcium gluconate | DNIs: bisphosphonates, calcitonin, Lasix, phenytoin |
| Iron | Microcytic anemia, pica, pallor, fatigue, cheilosis, glossitis, koilonychia, poor pregnancy outcomes | Low gastric acid, malabsorptive disorders, kidney dysfunction, poor intake | 150-200 mg/d elemental iron; take with vitamin C | DNIs: PPIs, OC, oral bisphosphonates, phosphate biners, fiber, levothyroxine ↓ absorption |
| Magnesium | Tetany, Chvostek and Trousseau signs, arrhythmias | Critical illness, malabsorptive disorders, EtOH abuse, AKD/CKD |
Laboratory values: 1-1.5 = 2-4 g Mg sulfate; <1 = 4-10 g Mg sulfate |
DNIs: platin-based chemotherapy agents, thiazide/loop diuretics ↓ K+/Ca2+ refractory to treatment until Mg levels corrected; ↓ levels with refeeding syndrome |
| Potassium | Weakness, lethargy, muscle necrosis, arrhythmias | Poor intake, AKD/CKD, malabsorptive disorders, hypermetabolic/refeeding syndrome, diabetes insipidus |
Oral: 40-100 mEq/d IV: 10-20 mEq/h depending on severity of ↓ levels |
DNIs: diuretics, platin-based chemotherapy agents, insulin |
| Sodium | Headache, nausea, vomiting, muscle cramps, disorientation | Elderly (deficiency), starvation, PN populations | Based on clinical status | Laboratory values are affected by hydration status |
| Zinc | Poor wound healing, rash, alopecia, impaired night vision, alterations in taste and smell | Poor intake, alcohol abuse, wound healing/wound drainage, malabsorptive disorders, liver disease and macular degeneration | Wound healing: 220 mg BID for 10 days; macular degeneration: 80 mg/d | DNIs: phosphate binders, fiber ↓ absorption; corticosteroids and propofol ↑ urinary excretion |
| Copper | Anemia unresponsive to iron supplementation | Neonates fed cow’s milk, malnourished, malabsorptive syndromes, individuals taking high doses of zinc for 6-10 weeks | 2-4 mg/d | Deficiency is rare in healthy individuals |
| Iodine | Goiter, hypothyroidism | Pregnant women who don’t consume dairy products; vegans; individuals not using iodized salt | 150-1,100 mcg/d | Pregnant women should take a daily prenatal supplement with 150 mcg |
| Manganese | Evidence is limited, but deficiency maybe linked to poor growth in children, skin rashes, hair depigmentation, poor bone health | No known populations are at risk | Insufficient data because deficiency is very rare |
Deficiency is very rare Individuals with liver dysfunction are at an increased risk for toxicity |
| Selenium | Keshan disease (cardiomyopathy), Kashin-Beck disease, male infertility, muscular weakness | Malnourished, dialysis, bariatric surgery, GI disorders, and individuals with diet-associated conditions such as PKU | >90 mcg/d |
IV selenium may reduce mortality in septic patients in the ICU. High doses (>400 mcg/d) can be toxic. |
| Abbreviations: AKD = acute kidney disease; BID = twice a day; Ca2+ = calcium; CKD = chronic kidney disease; d = day; DNI = drug-nutrient interaction; EtOH = ethanol; g = gram; GI = gastrointestinal; h = hour; ICU = intensive care unit; IV = intravenous; K+ = potassium; mcg = microgram; mEq = milliequivalent; Mg = magnesium; mg = milligram; OC = oral contraceptive; PKU = phenylketonuria; PN = parenteral nutrition; PPI = proton-pump inhibitor. | ||||
Micronutrient Deficiencies
Reportedly affecting more than 2 billion people worldwide, the deficiency of micronutrients has been described as the “hidden hunger”31 and can be caused by a multitude of factors. However, because most Americans do not follow the Dietary Guidelines recommendations, poor dietary habits are likely 1 of the primary contributors to inadequate intake.
Worldwide, deficiencies of vitamin A, iron, zinc, folate, and iodine reportedly are the most common.32 Data from the National Health and Nutrition Examination Survey (NHANES) 2005-2016 What We Eat in America survey data noted that in addition to inadequate vitamin A intake (45%), insufficient intakes of vitamins C (46%), D (95%), and E (84%) were also common in the US population when only food intake was evaluated. Inadequate zinc intake was also reported in 15% of the surveyed study participants.32 Although inadequate intake was also described for other micronutrients such as vitamin B6 (11%), folate (12%), and iron (5%), insufficiencies of these micronutrients are less common.32
Dietary supplements have led to a reduction in nutrient inadequacy. When the use of dietary supplements was evaluated in addition to food intake, inadequacies were reduced as follows: vitamin A from 45% to 35%; vitamin C, 46% to 33%; vitamin D, 95% to 65%; vitamin E, 84% to 60%; and zinc, 15% to 11%.32
Check your understanding with the following case study activity:
In addition to the aforementioned variety of factors that can affect micronutrient need and availability, many other factors, such as food choices, food preparation, food plantings and harvesting, and climate change, also have an impact.
Food Choices
“No one size fits all” when it comes to what consumers eat, because there are many reasons why people choose to eat what they do (see chapter 3 for a more in-depth discussion). Popular diets such as low-carbohydrate (low carb), high-protein, or the ketogenic (“keto”) diet (high fat and low carb) are often the focus of “healthy eating.” Moreover, dietary restrictions such as reduced sodium, potassium, or phosphorus may be prescribed based on one’s health status.
Conversely, the national and global dietary recommendations for health and wellness promote a plant-based, whole-foods approach that reflects an intake of a variety of foods that provide not only macronutrients but also important micronutrients and phytonutrients. Examples include the DASH and the Mediterranean diet. Both are evidence-based approaches to preventing and managing diet-related medical conditions.33,34
These “diets” share similar characteristics in their fundamental principles. Both promote the intake of a variety of fruits, vegetables, unprocessed whole grains, legumes, nuts, seeds, and healthy fats, which provide an array of valuable micronutrients including antioxidants along with phytonutrients. Together, these have a synergistic effect that reduces blood glucose, serum lipid, and inflammatory biomarker levels, thereby promoting disease prevention and management.35 Animal proteins, processed foods, and alcohol are recommended to be consumed less often.
These recommendations contrast with what the average American is reportedly consuming. Most don’t meet the guidelines for fruit and vegetable consumption: only 1 in 10 Americans consumes the recommended servings per day.32 Additionally, most Americans don’t meet the guidelines of 2 to 3 servings per day for dairy intake, although intake of calcium-fortified dairy alternatives can help people meet the RDA for calcium.
Impact of Popular Diets on Micronutrient Intake
In recent years, multiple different eating patterns with distinct attributes have been popularized and followed by American adults. Each dietary pattern may affect micronutrient status. Therefore, understanding the relationship between these diets and micronutrient intake is essential to ensure optimal nutritional and health status. The following discussion reviews selected popular diets, their attributes, and their potential impact on micronutrient excess or deficiency.36 For more information, refer to chapter 8, which reviews popular diets in more detail. Table 5.10 provides a summary of popular diets and their impact on micronutrient status.
Vegetarian-Style Diets
- Lacto-ovo-vegetarian:
- Attributes: Excludes meat, poultry, and fish but may include dairy (lacto-vegetarian) and egg (ovo-vegetarian) products.
- Impact on micronutrient status: Lacto-ovo-vegetarians may be at risk for deficiencies in vitamin B12, iron, zinc, and omega-3 fatty acids.
- Supplementation: Vitamin B12 supplementation is often recommended for vegetarians to meet their needs.
- Vegan diet:
- Attributes: Excludes all animal products, including meat, fish, eggs, dairy, and honey. Products that may involve animal products or wildlife, such as certain beers or figs, may be excluded too.
- Impact on micronutrient status: Vegans commonly face potential deficiencies in vitamin B12, iron, calcium, iodine, zinc, and omega-3 fatty acids.
- Supplementation: Vitamin B12, iron, and omega-3 fatty acid supplementation are often advised for vegans. Calcium and iodine sources should also be carefully considered.
Pescatarian Diet
-
- Attributes: Excludes meat and poultry but includes fish and other seafood.
- Impact on micronutrient status: Pescatarians generally have a lower risk of deficiencies compared with vegetarians because they consume seafood. Seafood provides essential nutrients such as omega-3 fatty acids, vitamin B12, and iron.
- Supplementation: Depending on individual dietary choices, supplementation may still be necessary, particularly for vitamin D and omega-3 fatty acids.
Paleolithic Diet (Paleo)
-
- Attributes: Emphasizes whole foods, lean meats, fish, fruits, vegetables, nuts, and seeds while excluding refined grains, legumes, dairy, and processed foods.
- Impact on micronutrient status: The paleo diet may result in inadequate intakes of calcium, vitamin D, vitamin E, and some B vitamins.
- Supplementation: Depending on individual dietary choices and sun exposure for vitamin D synthesis, supplementation may be needed for certain nutrients.
Low-Carbohydrate Diets
- Ketogenic diet (keto)
- Attributes: High fat, very low carbohydrate, and moderate protein intake; emphasizes intake of nuts and seeds, red meat, poultry, fish and seafood, eggs, full-fat dairy, and oils.
- Impact on micronutrient status: The keto diet may lead to deficiencies in fiber, vitamin C, vitamin D, vitamin E, vitamin K, calcium, magnesium, potassium, and some B vitamins due to the limited variety of food choices.
- Supplementation: Supplementation with vitamins and minerals, particularly those mentioned, may be necessary to avoid potential deficiencies.
- Low-carbohydrate/high-protein diet
- Attributes: Restricts carbohydrate intake while emphasizing high protein consumption.
- Impact on micronutrient status: Low-carb/high-protein diets may lead to deficiencies in vitamins C, D, and E; folate; calcium; magnesium; and potassium, due to limited intake of fruits, vegetables, and whole grains.
- Supplementation: Consideration should be given to supplementation, especially for vitamins and minerals commonly found in plant-based foods.
Check your understanding with the following activity:
Table 5.10. Summary of Popular Diets Defining Features and Impact on Micronutrient Status36
| Vegetarian-style diet | Defining feature |
Impact on micronutrient status |
Possible supplementation needed |
|---|---|---|---|
| Lacto-ovo-vegetarian | Plant-based foods, excluding meat and fish | Potential deficiency in vitamin B12, iron, zinc, and omega-3 fatty acids | Vitamin B12, iron |
| Pescatarian | Includes fish, excludes meat and dairy products | Reduced risk of deficiencies compared with vegetarian | Vitamin B12 |
| Vegan | Excludes all animal products | Potential deficiencies in vitamin B12, iron, calcium, and omega-3s | Vitamin B12, iron, calcium, omega-3s |
| Ketogenic | High fat, very low carbohydrate intake | Possible deficiency in vitamins C, D, E; calcium; and magnesium | B vitamins, vitamins C, D, E; calcium and magnesium |
| Paleo | Emulates ancestral diets | Potential deficiency in calcium, vitamin D, fiber | Vitamin D and calcium |
| Low-carb/ high-protein | Low carbohydrate, high protein intake | Potential deficiency in B vitamins and vitamin C | B vitamins and vitamin C |
Food Production and Harvesting: How It Affects Micronutrient Availability
The essence of food production depends on the quality of the soil food is grown in as plants extract nutrients from the soil. This makes up the nutrient composition of the plant.
The nutrients obtained from eating chicken, beef, and pork also contribute to a nutrient-dense diet based on the nutrient availability and micronutrient density in these animals’ feeds. Nutrients are returned to the soil through organic matter (plant or livestock biomatter), in addition to the use of inorganic fertilizers. These avenues are essential to maintain or replenish the fertility of the soil. However, the refurbishing of these nutrients rarely fully replaces all that are lost; thus, over time, harvesting results in continued soil nutrient loss. Furthermore, soil nutrient content is variable from region to region throughout the world. Although increased global food production and distribution have reduced some nutritional deficiencies, micronutrient deficiencies related to iron, calcium, zinc, and vitamin A still occur. Lower soil levels of zinc, copper, and manganese have been associated with increased child mortality.37 And micronutrient deficiencies arising from consumption of nutrient-poor foods also can adversely affect childhood and adolescent growth.38
Reportedly, soil degradation affects most of the global food production regions.37 To meet the global need for food in 2050, it is estimated that food production will need to increase by 70% to 100% of today’s production.39 To promote and maintain optimal food production that will produce high nutritional quality food to meet the nutritional needs of the world’s population, including provision of essential micronutrients, soil management is crucial in agriculture. Farming practices that focus solely on increasing yield often lead to lower micronutrient content of the crop.
Global trade of food has led to an increased allocation in the variety of foods available across the world. Although this has led to an increased availability of foods, the availability of nutrient-rich foods may not be equitable. For example, refined wheat products may be fortified with micronutrients lost in processing in some countries, but not all. Fortification typically depends on the economic state of the country. Higher-income countries are more likely to fortify products that have been stripped of their micronutrients.
Increasing global trade of food increases the exposure of the world’s population to foods grown in nutrient-poor soils. Food is highly perishable and prone to damage from pests and nutrient degradation during post-farm production handling, transportation, storage, and packaging. These aggregated factors lead to the consumption of nutrient-poor foods, which can lead to malnutrition and diet-related health consequences.
Farming Practices
Farming practices also play a critical role in the micronutrient content of plants and livestock. Nutrient density is dropping in harvested crops due to over-tilling, use of nitrogen fertilizers, focusing on increased yield, using synthetic pesticides, and other factors. However, implementing regenerative farming practices (replenishing soil organic matter and health), also known as “conservative agriculture,” can result in higher levels of micronutrients and phytonutrients.40
Instituting regenerative farming practices improves soil health and plant micronutrient content at farms where traditional practices previously were used. In addition, regenerative farming practices also led to an increase in omega-3 fatty acid levels in meat when compared with meat from grass-fed animals, using conventional farming.40
Climate Change
Climate change also can have a significant impact on soil nutrient density. Crops grown in regions with higher carbon dioxide (CO2) levels reportedly have 3% to 17% less iron, zinc, and protein.41 Lower protein content in wheat, potatoes, barley, and rice are projected to decline 6% to 14% if atmospheric CO2 levels continue to increase.42 Reduced amounts of several B vitamins, iron, and zinc have been found in different varieties of rice, due to higher levels of CO2 as well.
Micronutrient Dietary Excesses
Despite popular belief that more is better, excessive intake of several micronutrients may be associated with adverse health outcomes. Food choices such as overconsumption of prepared and fast foods increase sodium intake. Excess fluoride intake during critical periods of tooth formation can be detrimental. Furthermore, increased intake of potassium and phosphorus by patients with chronic kidney disease can increase their risk for morbidity and death. Lastly, dietary supplements are commonly used and contribute, in addition to diet, to the overall intake of micronutrients—something most consumers don’t consider.
The FDA reports adults in the United States consume 3,400 mg of sodium daily, which exceeds the recommendations set forth by the Dietary Guidelines of ≤2,300 mg/d.43 Furthermore, the American Heart Association recommends ≤1,500 mg/d for adults with hypertension. It is concerning, then, that reportedly 40% of US adults, including almost 60% of non-Hispanic Black people, have hypertension related to excessive sodium intake.44 Moreover, hypertension may increase the risk for heart disease and stroke, primary causes of death. Processed, packaged, and ready-prepared foods contribute the majority of dietary sodium intake.43 Numerous low-sodium options are available, and their use should be encouraged to reduce intake, in addition to following the DASH or Mediterranean dietary patterns to promote risk reduction.45
Beginning in the mid-1940s, a large proportion of the water in the United States has been supplemented with fluoride, based on observations that dental caries were significantly lower in populations drinking water with higher fluoride concentrations. Today, approximately 60% of the US population consumes water from community sources that is fortified with fluoride as a public health measure to reduce the prevalence of dental caries.46 Note that bottled water, increasingly consumed by adults, is generally a relatively poor source of fluoride. Although fluoridation of water sources has reduced the prevalence of dental caries in the United States, excess intake of fluoride can lead to dental fluorosis, which occurs when the tooth is developing during the first 8 years of life. Excess fluoride after this time will not have any adverse effects on the teeth.46
Using NHANES data from 2011 to 2014, Cowan et al.47 found that surveyed participants ≥19 years of age who used dietary supplements exceeded the recommended intake levels for iron, folic acid, vitamin D, and calcium, regardless of their living situations and health status. This, in turn, could lead to adverse outcomes. See chapter 6 for a detailed discussion on dietary supplements.
Several medical conditions, including hemochromatosis and chronic kidney disease, may require restricting micronutrient intake to avoid the adverse effects of overconsumption. For example, in hemochromatosis, iron intake is restricted to prevent excess iron storage in the liver, heart, and pancreas. Excess storage can eventually cause liver, cardiac, and pancreatic failure. Individuals with chronic kidney disease are often counseled to limit their intake of potassium and phosphorus to avoid adverse effects of hyperkalemia and hyperphosphatemia that occur due to compromised renal excretion. Excess intake of vitamin E and calcium also have been linked to an increased risk for prostate cancer in men, with recommendations focused on not exceeding the recommended daily intake levels.48
Summary
Although micronutrients are required in small amounts by the body, they are vital for promoting and maintaining health and wellness. Many factors can alter an individual’s micronutrients requirements and status. Dietary choices, health status, availability of and access to healthy foods, and food production methods from farming to processing influence the micronutrient content in the foods we eat and, ultimately, micronutrient status.
By completing a comprehensive nutrition assessment that includes an evaluation of weight history and body composition, available laboratory data, past and present medical status, and dietary habits, individuals with or at risk for developing micronutrient deficiencies can be identified. A nutrition-focused physical exam provides additional data on whether any signs of deficiencies are present.
Subsequently, appropriate counseling can then help prevent deficiencies or maintain or improve micronutrient status. Evaluating current status and risk for deficiency can help prevent or manage medical conditions or diseases associated with various micronutrients.
Consuming plant-based diets such as the DASH or Mediterranean-style diet can provide a rich foundation for micronutrients intakes. These diets also reduce the diet-related diseases of heart disease, stroke, type 2 diabetes, and hypertension. Overall, understanding the factors affecting micronutrient intake can lead to improved, evidenced-based nutrition counseling and intervention.
Practice Case
Andrea is a 23-year-old woman who changed her eating habits 6 months ago because she wanted to become a vegan and heard that the vegan diet was heathier. She’s made an appointment with you because she feels tired and weak often. She also tells you she’s having trouble concentrating, is dizzy at times, and she can feel some tingling in her feet.
You notice her skin looks pale and her tongue is smooth and red.
Diet History
- Breakfast: ½ cup of oatmeal with honey, almonds, and apples. 8 oz of black coffee
- Morning snack: ½ cup of edamame
- Lunch: 1 cup of kale and quinoa salad, lemon vinaigrette dressing; 8 oz of fruit smoothie
- Afternoon snack: handful of pita chips with hummus
- Dinner: lentil soup, small garden salad (mixed greens, olives, vegan feta cheese, and tomatoes), and 2 slices of sourdough bread
- Dessert: fruit sorbet
Patient history: gastrointestinal reflux disease
Medication: proton-pump inhibitor
Laboratory values:
- MCV: 105 femtoliters (fL; normal range: 80-100 fL)
- Hemoglobin: 12.8 g/dL (normal range: 14-18 g/dL)
Using the information about Andrea in the preceding practice case, test your understanding by answering the questions in the following activities:
Key Takeaways
- Micronutrients include a variety of vitamins and minerals that are needed in small amounts but are essential for health and wellness.
- Several factors can influence micronutrient intake, including appetite, source of nutrition, health status, type of food consumed, and method of food preparation.
- Dietary patterns, following trendy diets, and use of dietary supplements can lead to excessive or insufficient micronutrient intake.
- Commonly used medications can increase the risk for micronutrient deficiencies. Education is often needed to help patients minimize that risk.
- Micronutrient deficiencies can be detected by completing a nutrition-focused physical exam and the use of biomarkers.
References
- National Institutes of Health Office of Dietary Supplements. Nutrient recommendations and databases. Accessed May 12, 2023. https://ods.od.nih.gov/HealthInformation/nutrientrecommendations.aspx
- DRI calculator for healthcare professionals. National Agriculture Library, US Department of Agriculture. Accessed May 12, 2023. https://www.nal.usda.gov/human-nutrition-and-food-safety/dri-calculator
- How to understand and use the Nutrition Facts label. US Food and Drug Administration. Accessed May 12, 2023. https://www.fda.gov/food/new-nutrition-facts-label/how-understand-and-use-nutrition-facts-label#:~:text=The%20Daily%20Values%20are%20reference,or%20low%20in%20a%20nutrient.
- The lows and highs of percent daily value on the new Nutrition Facts label. US Food and Drug Administration. Accessed June 26, 2023. https://www.fda.gov/food/new-nutrition-facts-label/lows-and-highs-percent-daily-value-new-nutrition-facts-label
- Drake VJ. Thiamin. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated October 2021. Accessed May 13, 2023. https://lpi.oregonstate.edu/mic/vitamins/thiamin
- Drake VJ. Riboflavin. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated July 2022. Accessed May 13, 2023. https://lpi.oregonstate.edu/mic/vitamins/riboflavin
- Delage B. Niacin. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated August 10, 2018. Accessed June 21, 2023. https://lpi.oregonstate.edu/mic/vitamins/niacin.
- Johnson LE. Vitamin B6 deficiency and dependency. Merck Manual professional version. November 2022. Accessed June 21, 2023. https://www.merckmanuals.com/professional/nutritional-disorders/vitamin-deficiency,-dependency,-and-toxicity/vitamin-b6-deficiency-and-dependency
- Drake VJ. Vitamin B12. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated June 4, 2015. Accessed June 21, 2023. https://lpi.oregonstate.edu/mic/vitamins/vitamin-B12
- Drake VJ. Folate. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated December 2014. Accessed June 21, 2023.https://lpi.oregonstate.edu/mic/vitamins/folate
- Delage B. Vitamin C. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated December 2018. Accessed June 21, 2023. https://lpi.oregonstate.edu/mic/vitamins/vitamin-C
- Drake VJ. Pantothenic acid. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated July 2015. Accessed June 21, 2023. https://lpi.oregonstate.edu/mic/vitamins/pantothenic-acid
- Drake VJ. Biotin. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated March 2023. Accessed June 21, 2023. https://lpi.oregonstate.edu/mic/vitamins/biotin
- Drake VJ. Vitamin A. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated February 25, 2021. Accessed June 22, 2023. https://lpi.oregonstate.edu/mic/vitamins/vitamin-A
- Delage B. Vitamin D. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated February 11, 2021. Accessed June 22, 2023. https://lpi.oregonstate.edu/mic/vitamins/vitamin-D
- Delage B. Vitamin E. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated October 2015. Accessed June 22, 2023. https://lpi.oregonstate.edu/mic/vitamins/vitamin-E
- Drake VJ. Vitamin K. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated July 2022. Accessed June 22, 2023. https://lpi.oregonstate.edu/mic/vitamins/vitamin-K
- Bielik V, Kolisek M. Bioaccessibility and bioavailability of minerals in relation to a healthy gut microbiome. Int J Mol Sci. 2021;22(13):6803. doi:10.3390/ijms22136803
- Delage B. Calcium. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated September 2017. Accessed June 22, 2023. https://lpi.oregonstate.edu/mic/minerals/calcium
- Delage B. Iron. Linus Pauling Micronutrient Information Center. Updated May 2016. Accessed June 22, 2023. https://lpi.oregonstate.edu/mic/minerals/iron
- Delage B. Magnesium. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated February 2019. Accessed June 23, 2023. https://lpi.oregonstate.edu/mic/minerals/magnesium
- Delage B. Potassium. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated April 2019. Accessed June 23, 2023. https://lpi.oregonstate.edu/mic/minerals/potassium
- Delage B. Sodium (chloride). Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated April 11, 2019. Accessed June 23, 2023. https://lpi.oregonstate.edu/mic/minerals/sodium
- Delage B. Zinc. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated May 2019. Accessed June 23, 2023. https://lpi.oregonstate.edu/mic/minerals/zinc
- Collins JF. Copper. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated January 2014. Accessed June 23, 2023. https://lpi.oregonstate.edu/mic/minerals/copper
- Drake VJ. Iodine. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated January 2014. Accessed June 23, 2023. https://lpi.oregonstate.edu/mic/minerals/iodine
- Drake VJ. Manganese. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated May 2021. Accessed June 23, 2023. https://lpi.oregonstate.edu/mic/minerals/manganese
- Drake VJ. Selenium. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated June 2015. Accessed June 23, 2023. https://lpi.oregonstate.edu/mic/minerals/selenium
- Drake VJ. Molybdenum. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated May 2021. Accessed June 23, 2023. https://lpi.oregonstate.edu/mic/minerals/molybdenum
- Drake VJ. Fluoride. Oregon State University Linus Pauling Institute, Micronutrient Information Center. Updated December 2021. Accessed June 25, 2023. https://lpi.oregonstate.edu/mic/minerals/fluoride
- Lowe NM. The global challenge of hidden hunger: perspectives from the field. Proc Nutr Soc. 2021;80(3):283-289. doi: 10.1017/S0029665121000902
- Reider CA, Chung RY, Devarshi PP, Grant RW, Mitmesser SH. Inadequacy of immune health nutrients: intakes in US adults, the 2005-2016 NHANES. Nutrients. 2020;12(6):1735. doi:10.3390/nu12061735
- Wang JS, Liu WJ, Lee CL. Associations of adherence to the DASH diet and the Mediterranean diet with all cause mortality in subjects with various glucose regulation states. Front Nutr. 2022;9:828792. doi:10.3389/fnut.2022.828792
- Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001; 344:3–10. doi:10.1056/NEJM200101043440101
- Koelman L, Rodrigues CE, Aleksandrova K. Effects of dietary patterns on biomarkers of inflammation and immune responses: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr. 2022;13(1):101-115. doi:10.1093/advances/nmab086
- Tahreem A, Rakha A, Rabail R, et al. Fad diets: facts and fiction. Front Nutr. 2022;9:960922. doi:10.3389/fnut.2022.960922
- Silver WL, Perez T, Mayer A, Jones AR. The role of soil in the contribution of food and feed. Philos Trans R Soc Lond B Biol Sci. 2021;376(1834):20200181. doi:10.1098/rstb.2020.0181
- Berkhout ED, Malan M, Kram T. Better soils for healthier lives? An econometric assessment of the link between soil nutrients and malnutrition in Sub-Saharan Africa. PLoS One. 2019;14,2-3. doi:10.1371/journal.pone.0210642
- Global Panel. Healthy diets for all: a key to meeting the SDGs. Policy Brief No. 10. Global Panel on Agriculture and Food Systems for Nutrition; 2017
- Montgomery DR, Biklé A, Archuleta R, Brown P, Jordan J. Soil health and nutrient density: preliminary comparison of regenerative and conventional farming. PeerJ. 2022;10:e12848. doi:10.7717/peerj.12848
- Smith P, Haberl H, Popp A, et al. How much land‐based greenhouse gas mitigation can be achieved without compromising food security and environmental goals? Glob Chang Biol. 2013;19(8):2285-2302. doi:10.1111/gcb.12160
- Semba RD, Askari S, Gibson S, Bloem MW, Kraemer K. The potential impact of climate change on the micronutrient-rich food supply. Adv Nutr. 2022;13(1):80-100. doi:10.1093/advances/nmab104
- Sodium reduction in the food supply. US Food and Drug Administration. Updated September 3, 2024. Accessed December 20, 2024. https://www.fda.gov/food/food-additives-petitions/sodium-reduction
- How much sodium should I eat a day? American Heart Association. Updated November 1, 2021. Accessed June 30, 2023. https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/sodium/how-much-sodium-should-i-eat-per-day
- De Pergola G, D’Alessandro A. Influence of Mediterranean diet on blood pressure. Nutrients. 2018;10(11):1700. doi:10.3390/nu10111700
- About community water fluoridation. Centers for Disease Control and Prevention. Updated May 15, 2024. Accessed October 31, 2024. https://www.cdc.gov/fluoridation/about/?CDC_AAref_Val=https://www.cdc.gov/fluoridation/basics/index.htm
- Cowan AE, Jun S, Tooze JA, et al. Total usual micronutrient intakes compared to the dietary reference intakes among U.S. adults by food security status. Nutrients. 2020;12(1):38. doi:10.3390/nu12010038
- Klein EA, Thompson IM Jr, Tangen CM, et al. Vitamin E and the risk of prostate cancer: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA. 2011;306(14):1549-1556. doi:10.1001/jama.2011.1437
Vitamins, minerals, and trace elements required in small quantities. They support various bodily functions and are essential for growth and development.
Essential micronutrients, broadly categorized into water-soluble or fat-soluble vitamins.
Inorganic substances that are essential for the body’s proper functioning, including elements such as calcium, iron, zinc, and magnesium.
Minerals that are required by the body in very small amounts. Examples include iron, zinc, copper, selenium, and iodine.
Inadequate nutrient intake or absorption that can lead to specific health problems or diseases.
A set of scientifically developed reference values for nutrients. Source: US Department of Health and Human Services
A recommended average daily intake level for a nutrient when there is not enough scientific evidence to establish an RDA. Source: National Institutes of Health
The average daily intake of a nutrient estimated to meet the requirements of half the healthy individuals in a particular life stage and gender group. Source: National Institutes of Health
The average daily intake of a nutrient that is sufficient to meet the requirements of most healthy individuals in a particular life stage and gender group. Source: National Institutes of Health
The highest level of daily nutrient intake that is unlikely to cause adverse health effects in almost all individuals. Source: Scientific Committee on Food
One value for each nutrient, selected for the labels of dietary supplements and food. It is often, but not always, similar to one’s RDA or AI for that nutrient. Source: National Institutes of Health
Vitamins that dissolve in fat and can be stored in the body's fatty tissues, including vitamins A, D, E, and K. Source: Human Nutrition
Vitamins that dissolve in water and are not stored in the body for long periods. These include vitamin C and B-complex vitamins. Source: Human Nutrition
Lipids that are liquid at room temperature. Source: Nutrition Concepts and Controversies, 15th Edition
Any of the ions (as of sodium or calcium) that in biological fluid regulate or affect most metabolic processes (such as the flow of nutrients into and waste products out of cells). Source: Merriam-Webster Online Dictionary
A common chronic infectious disease resulting from tooth-adherent bacteria that metabolize sugars to produce acid, which, over time, demineralizes tooth structure. Source: National Library of Medicine
A Chinese cabbage forming an open head with long white stalks and green leaves. Source: Merriam-Webster Online Dictionary
A product consumed in addition to a regular diet to supplement the intake of certain nutrients, available in various forms, such as pills, capsules, powders, and liquids. Source: US Food and Drug Administration
Compounds produced by plants that provide health benefits to the body. Also called phytochemicals or antioxidants. Source: US Department of Agriculture’s National Agriculture Library
A group of compounds composed of oxygen, hydrogen, and carbon atoms that supply the body with energy. Source: Merriam-Webster Online Dictionary
One class of polyunsaturated fatty acids with 3 double bonds. They're present in foods such as flaxseed, walnuts, and fatty fish used to make eicosanoids and are associated with decreasing inflammation. Source: Nutrition Concepts and Controversies, 15th Edition
A common disorder characterized by hypomineralization of tooth enamel caused by the excessive ingestion of fluoride during tooth development. Source: National Library of Medicine

