Sarah Grace
What is Advance Care Planning?
Advance care planning is the process of thinking about and documenting one’s preferences for future medical care, particularly in situations where an individual may become unable to communicate their decisions due to illness or incapacity.
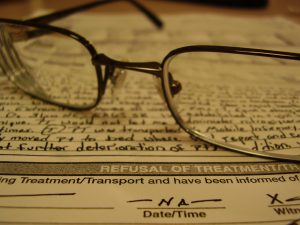
It typically involves completing legal documents, such as living wills and durable powers of attorney for healthcare, which specify the types of medical treatments a person would or would not want and appoint a healthcare proxy to make decisions on their behalf.
The goal of advance care planning is to ensure that an individual’s wishes are respected during end-of-life care or during critical medical situations, providing peace of mind for both the individual and their loved ones.
What is involved with creating an Advance Care Plan?
Creating an advance care plan involves several key steps to ensure that an individual’s healthcare preferences are clearly documented and respected in the event that they are unable to make decisions for themselves. The specifics of this process include:
- Reflecting on Personal Values and Preferences:
The first step in creating an advance care plan is personal reflection. Individuals need to think about their values, beliefs, and what they consider to be an acceptable quality of life. This includes decisions about life-sustaining treatments, such as mechanical ventilation, tube feeding, and resuscitation. Reflecting on these questions helps individuals understand what they would want in different medical scenarios (Institute of Medicine, 2015). - Discussing Wishes with Loved Ones and Healthcare Providers:
Open communication with family members, loved ones, and healthcare providers is a critical part of advance care planning. These conversations ensure that others are aware of the individual’s wishes and can help facilitate decision-making if needed. A healthcare provider may provide guidance on specific medical scenarios and the likely outcomes of various treatment options (Sudore & Fried, 2010). - Completing Legal Documents:
Advance care planning typically includes completing two key legal documents:- Living Will: This document specifies what kinds of medical treatment the individual would or would not want if they become incapacitated. It addresses decisions like whether to use life support, dialysis, or artificial nutrition.
- Durable Power of Attorney for Healthcare (Healthcare Proxy): This document appoints someone to make healthcare decisions on the individual’s behalf if they are unable to do so. The healthcare proxy should be someone the individual trusts to carry out their wishes (American Bar Association, 2020).
- Reviewing and Updating the Plan:
Advance care plans should be revisited periodically, especially after significant life events such as a new diagnosis, changes in health status, or shifts in personal beliefs. Keeping the plan updated ensures that it continues to reflect the individual’s current wishes (National Institute on Aging, 2021). - Ensuring Accessibility of Documents:
Once completed, it’s important that the individual ensures their documents are easily accessible. Copies should be shared with the healthcare proxy, family members, and healthcare providers. Some states in the U.S. allow individuals to register their advance directives in state databases to ensure they are available when needed (Sudore & Fried, 2010).
What are the Benefits of Having an ACP?
Having an advance care plan offers several important benefits for both individuals and their loved ones, particularly when facing serious illness or end-of-life situations. These benefits include:
1. Ensures Alignment with Personal Wishes
One of the most significant benefits of an advance care plan is that it ensures that an individual’s healthcare preferences are followed, even when they are no longer able to communicate their wishes. By specifying preferred medical treatments, or the lack thereof, individuals can have peace of mind that they will receive care that aligns with their values and beliefs. Studies show that individuals who complete advance care planning feel a greater sense of control over their future healthcare, reducing anxiety and uncertainty (Detering et al., 2010).
2. Reduces Stress and Conflict for Loved Ones
When an individual does not have an advance care plan, family members are often left to make difficult healthcare decisions during emotionally charged moments. This can lead to family conflict and significant stress for loved ones, especially if they are unsure of the patient’s wishes. An advance care plan can prevent these conflicts by clearly outlining the individual’s preferences, thereby lifting the emotional burden from family members. Families who are informed about the patient’s preferences are more likely to experience less guilt and emotional distress when making decisions (Detering et al., 2010).
3. Facilitates Better Communication with Healthcare Providers
An advance care plan fosters better communication between patients and healthcare providers. When providers are aware of an individual’s preferences for treatment, they can make informed medical decisions that respect those choices. This improves the quality of care by aligning medical interventions with the patient’s wishes, often resulting in care that is more focused on comfort and quality of life, rather than unnecessary or unwanted aggressive treatments (Brinkman-Stoppelenburg, Rietjens, & van der Heide, 2014).
4. Improves End-of-Life Care
Research has found that advance care planning significantly improves the quality of end-of-life care. Individuals who have clear directives are more likely to receive care in accordance with their preferences, including palliative care, hospice, or comfort-focused care. These patients often experience less invasive treatments and are more likely to die in their preferred location, whether at home or in a hospice setting, rather than in a hospital with intensive interventions (Brinkman-Stoppelenburg et al., 2014).
5. Reduces Unnecessary Healthcare Costs
Another benefit of advance care planning is the potential reduction of unnecessary healthcare interventions, particularly aggressive treatments that the patient might not have wanted. Studies have shown that individuals with advance care plans are less likely to receive life-sustaining treatments that do not improve their quality of life, leading to a decrease in costly and invasive procedures (Silveira, Kim, & Langa, 2010). This not only aligns with the patient’s preferences but also helps reduce the financial burden on families and the healthcare system.
The Role of Autonomy and Control in Advanced Directives
One of the most significant psychological motivations for creating an advanced directive is the desire for autonomy and control over one’s medical care. Research has shown that the act of completing an AD can provide individuals with a sense of empowerment and reduce anxiety about the future (Detering et al., 2010). This sense of control is particularly salient when individuals face the uncertainty of illness or the inevitability of death. From a psychological perspective, feeling in control of decisions about life-sustaining treatments, pain management, and the location of care (home vs. hospital) can alleviate some of the distress associated with dying.
However, the desire for control can be complicated by cognitive biases, such as the optimism bias, which leads individuals to overestimate the likelihood of favorable outcomes and avoid confronting the reality of their declining health (Sharot, 2011). Additionally, research indicates that individuals often delay making decisions about advanced directives, despite understanding their importance, because of avoidance behaviors associated with death anxiety (Pyszczynski et al., 2004). These emotional and cognitive factors often make discussions about advanced directives challenging for patients, families, and healthcare providers alike.
Click the link below to learn more about advanced care planning:
This video explains what is involved in advanced care planning:
References
American Bar Association. (2020). Giving someone a power of attorney for your health care. Retrieved from https://www.americanbar.org
Brinkman-Stoppelenburg, A., Rietjens, J. A., & van der Heide, A. (2014). The effects of advance care planning on end-of-life care: A systematic review. Palliative Medicine, 28(8), 1000-1025. https://doi.org/10.1177/0269216314526272
Detering, K. M., Hancock, A. D., Reade, M. C., & Silvester, W. (2010). The impact of advance care planning on end-of-life care in elderly patients: Randomised controlled trial. BMJ, 340, c1345. https://doi.org/10.1136/bmj.c1345
Institute of Medicine. (2015). Dying in America: Improving quality and honoring individual preferences near the end of life. National Academies Press.
National Institute on Aging. (2021). Advance care planning: Healthcare directives. U.S. Department of Health and Human Services. Retrieved from https://www.nia.nih.gov
Pyszczynski, T., Greenberg, J., Solomon, S., Arndt, J., & Schimel, J. (2004). Why do people need self-esteem? A theoretical and empirical review. Psychological Bulletin, 130(3), 435–468. https://doi.org/10.1037/0033-2909.130.3.435
Sharot, T. (2011). The optimism bias. Current Biology, 21(23), R941-R945.
Silveira, M. J., Kim, S. Y., & Langa, K. M. (2010). Advance directives and outcomes of surrogate decision making before death. New England Journal of Medicine, 362(13), 1211-1218. https://doi.org/10.1056/NEJMsa0907901
Sudore, R. L., & Fried, T. R. (2010). Redefining the “planning” in advance care planning: Preparing for end-of-life decision making. Annals of Internal Medicine, 153(4), 256-261. https://doi.org/10.7326/0003-4819-153-4-201008170-00008

