12.4 Psychological Therapies and Behavioral Interventions
Open Resources for Nursing (Open RN)
Untreated mental, emotional, and behavioral disorders in childhood are linked with long-term consequences such as poorer education outcomes, employment problems and difficulty maintaining social relationships. Early treatment of a child’s mental health or behavioral problems can reduce problems at home, in school, in forming friendships, and can promote healthy development into adulthood.[1] Treatments include psychological therapy, parent training in behavioral management, and behavioral interventions for the classroom, among others.
Psychological Therapies
Depending on the type and severity of the mental health disorder, psychological therapy for children may be used in combination with prescribed medication. Psychological therapy helps a child manage their symptoms so that they can function well at home, in school, and in their community. For example, cognitive-behavioral therapy (CBT) works well for children with disruptive behavior disorders, depression, and anxiety.
Psychotherapy is conducted by trained mental health professionals for children and can be done individually or in groups. Methods with children can include talking, playing, or other activities to help the child express feelings and thoughts. Therapists may also observe parents and children together and make suggestions for different ways to respond to disruptive behaviors.
See Table 12.1 for a list of psychological therapies considered effective for common conditions in children and adolescents[2][3]
Table 12.1 Psychological Therapies for Various Conditions in Children and Adolescents
| Therapies | Description | Indications |
| Cognitive-Behavioral Therapy (CBT)
|
Teaches clients how to correct cognitive errors in thinking (such as, “nothing ever goes right for me”) and coaches them to try different behaviors (i.e., behavioral activation) to lead to changes in how they feel.
Exposure and response prevention (ERP) is a form of CBT for the treatment of obsessive-compulsive disorder (OCD). |
Anxiety disorders
Depressive disorders Oppositional defiant disorder Eating disorders Substance use disorder Post-traumatic stress disorder |
| Dialectical Behavior Therapy (DBT) | Specialized version of CBT with skills groups (to teach problem-solving, emotional regulation, distress tolerance, and interpersonal effectiveness skills), as well as individual therapy sessions. Mindfulness and meditation are often encouraged. | Chronic and significant suicide ideation and/or self-harm |
| Family Therapy | Sessions that focus on the family relationship or interaction patterns that cause dysfunction and assist the family members to amend that pattern (rather than saying the problem resides within an individual). | Eating disorders
Conduct disorder Depressive disorders Substance use disorders |
| Group Therapy | Addresses interaction pattern problems while also providing disorder-specific support within a group of strangers having similar challenges. Peer-based learning can be uniquely effective. | Anxiety disorders |
| Behavioral Management Training | Also known as parent management training, these programs teach and encourage skillful parent or caregiver responses to challenging child behaviors. Read more in the “Behavioral Interventions” subsection below. | Oppositional defiant disorder
Conduct disorder |
| Social Skills Training | Variety of group and one-to-one techniques to teach basic behavioral and cognitive skills, reinforce prosocial behaviors, and teach social problem-solving. Group sessions are more beneficial than individual sessions because of peer learning influences. | Oppositional defiant disorder
Attention deficit hyperactivity disorder (ADHD) Anxiety disorders Depressive disorders Autism spectrum disorder |
| Relaxation Training | Biofeedback, deep breathing, progressive muscle relaxation, and mindfulness are examples of strategies to increase mind-body awareness and enhance the ability to effectively calm emotional reactions. | Anxiety disorders
Depressive disorders |
| Environmental Enrichment Therapy | Therapist or parent led delivery of enhanced sensory experiences that promote improved language skills, learning, mood, and social skills | Autistic spectrum disorder
Selected developmental disabilities |
| Motivational Interviewing (MI) | A specific type of therapeutic communication regarding health behaviors a client needs to change but has significant reluctance. It helps clients state their own reasons for changing behaviors, resolve their own ambivalence, and state actions they can take to change. | Substance use disorders |
Behavioral Interventions
Behavioral interventions reward desired behaviors and reduce maladaptive coping behaviors. Most child and adolescent treatment settings used structured programs to motivate and reward age-appropriate behaviors. For example, the point or star system may be used where the child receives points or stars for desired behaviors, and then specific privileges are awarded based on the points or stars earned each day.[4]
Functional Analysis of Behavior
Functional analysis is a strategy for preventing a recurring problematic behavior by first identifying why a behavior keeps recurring and then devising a plan to prevent recurrences. For example, a parent reports their young child “throws temper tantrums every time we go to the store.” The mental health therapist and parent analyze the behavior, the parent realizes they have been giving the child candy to halt the tantrums, which actually functions to reward the behavior and encourages it to happen again. If the parent were to stop delivering this unintentional reward, the tantrums would theoretically decrease. Alternatively, the parent may focus on avoiding re-exposing the child to a recognized trigger for the behavior, such as the candy aisle.[5]
Play Therapy
Children develop physically, intellectually, emotionally, and socially through play. Play therapy encourages children to express feelings such as anxiety, self-doubt, and fear through their natural play. It also allows them to work through painful or traumatic memories. For example, nurses often use dolls or other toys to help children work through feelings of fear prior to a medical procedure.[6] See Figure 12.5a[7] for an image of children with special needs playing at a school for autism.

Bibliotherapy
Bibliotherapy uses books to help children express feelings in a supportive environment, gain insight into feelings and behavior, and learn new ways to cope with difficult situations. When children listen to or read a story, they identify with the characters and experience a catharsis of feelings. Stories and books should be selected based on the child’s cognitive and developmental levels that reflect the situations or feelings the child is experiencing and their emotional readiness for the topic.[8] See Figure 12.5b[9] for an image of bibliotherapy.

Expressive Arts Therapy
Art provides a nonverbal method of expressing difficult or confusing emotions. Drawing, painting, and sculpting with clay are commonly used art therapies. Children who have experienced trauma often show the traumatic event in their drawing when asked to draw whatever they wish.[10]
Journaling
Journaling is an effective technique for older children and teenagers. Journaling is a tangible way to record emotions and begin dialogue with others. A daily journal is also helpful in setting goals and evaluating progress.[11]
Music Therapy
Music has been recognized for centuries as having healing power. Music therapy is an evidence-based approach to improve an individual’s physical, psychological, cognitive, behavioral, and social functioning when listening to music, singing, or moving to music.[12] See Figure 12.5c[13] for an image of music therapy.

Parent Training in Behavior Management
Parent training in behavior management includes teaching skills and strategies such as positive reinforcement, structure, and consistent discipline to manage their child’s behavior and help them succeed at school, at home, and in relationships.[14] See Figure 12.4[15] for an illustration of parent training in behavioral management.
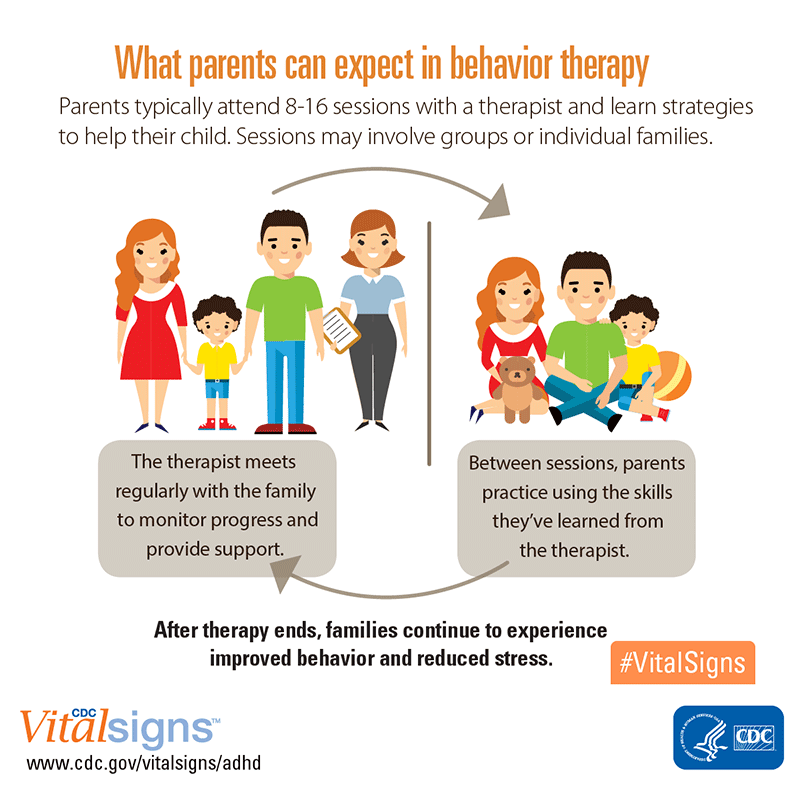
The therapist meets with the parents, patient, pertinent family members, and other caregivers as needed to observe the patient’s behaviors and to design strategies for problematic behaviors such as temper tantrums and aggression. There are generally eight or more sessions and parents practice techniques between appointments. The focus is on positive reinforcement for desirable behaviors along with clear guidelines for age-appropriate expectations and discipline [16] Several strategies that are used by nurses in inpatient settings can also be useful for parents and will be discussed in Chapter 12.5. These include using time-outs, scheduling special time, and establishing consistent sleep habits.
- Centers for Disease Control and Prevention. (2025, June 9). Treating children's mental health with therapy. www.cdc.gov/children-mental-health/treatment/?CDC_AAref_Val=https://www.cdc.gov/childrensmentalhealth/parent-behavior-therapy.html ↵
- Aronoff, E., Hillyer, R., & Leon, M. (2016). Environmental enrichment therapy for autism: Outcomes and increased access. Neural plasticity. 2016;2016:2734915. doi: 10.1155/2016/2734915. Epub 2016 Sep 18. PMID: 27721995; PMCID: PMC5046013.pmc.ncbi.nlm.nih.gov/articles/PMC5046013/ ↵
- Centers for Disease Control and Prevention. (2025, June 9). Treating children's mental health with therapy. www.cdc.gov/children-mental-health/treatment/?CDC_AAref_Val=https://www.cdc.gov/childrensmentalhealth/parent-behavior-therapy.html ↵
- Halter, M. (2022). Varcarolis’ foundations of psychiatric-mental health nursing (9th ed.). Saunders. ↵
- Psychology tools. (n.d). Functional analysis. In Psychology Tools. www.psychologytools.com/professional/techniques/functional-analysis ↵
- Halter, M. (2022). Varcarolis’ foundations of psychiatric-mental health nursing (9th ed.). Saunders. ↵
- “4885680339_721cd1843e_k” by World Bank Photo Collection is licensed under CC BY-NC-ND 2.0 ↵
- Halter, M. (2022). Varcarolis’ foundations of psychiatric-mental health nursing (9th ed.). Saunders. ↵
- “Bibliotherapy.jpg” by Shelley Rodrigo is licensed under CC BY 2.0 ↵
- Halter, M. (2022). Varcarolis’ foundations of psychiatric-mental health nursing (9th ed.). Saunders. ↵
- Halter, M. (2022). Varcarolis’ foundations of psychiatric-mental health nursing (9th ed.). Saunders. ↵
- Halter, M. (2022). Varcarolis’ foundations of psychiatric-mental health nursing (9th ed.). Saunders. ↵
- “103909417_f36b60ceec_k” by midiman is licensed under CC BY 2.0 ↵
- Hudson, J.L. et al. (2023). Interventions for young children's mental health: A review of reviews. Clinical child family psychological review,Jul 24;26(3) 593-641. doi: 10.1007/s10567-023-00443-6 ↵
- “adhd-behavior-therapy-parents-800px.png” by National Center on Birth Defects and Developmental Disabilities is in the Public Domain ↵
- Centers for Disease Control and Prevention. (2024, May 15). Parent training in behavior management for ADHD. Centers for Disease Control. www.cdc.gov/adhd/treatment/behavior-therapy.html ↵
Encourages children to express feelings such as anxiety, self-doubt, and fear through their natural play.
A behavioral intervention that uses books to help children express feelings in a supportive environment, gain insight into feelings and behavior, and learn new ways to cope with difficult situations.
An evidence-based approach to improve an individual’s physical, psychological, cognitive, behavioral, and social functioning when listening to music, singing, or moving to music.

