2.3 Trauma-Informed Care
Terri J. Farmer, PhD, PMHNP, CNE
Trauma has no age, gender, socioeconomic status, race, ethnicity, or sexual orientation boundaries. Many individuals experience trauma during their lifetimes that can have a lasting impact on their mental health. Trauma results from an event, series of events, or set of circumstances that are experienced by an individual as physically or emotionally harmful and can have lasting adverse effects on the individual’s functioning and physical, social, emotional, or spiritual well-being. Events may be human-made, such as war, terrorism, sexual abuse, violence, or they can be the products of nature (e.g., flooding, hurricanes, and tornadoes). Increasing research attention has been focused on the effects of healthcare interventions on trauma. For example, patients who have been hospitalized in ICUs are at risk for post-traumatic stress disorder. Nurses must keep in mind to not interject their own experiences or perspectives because something minor to them may be major to the patient.
It’s not just the event itself that determines if it is traumatic, but the individual’s experience of the event. Two people may be exposed to the same event or series of events but experience and interpret these events in vastly different ways. Various biopsychosocial and cultural factors influence an individual’s immediate response and long-term reactions to trauma. For most individuals, regardless of the severity of the trauma, the effects of trauma are met with resilience, defined as the ability to rise above circumstances or meet challenges with fortitude. Resilience includes the process of using available resources to negotiate hardship and/or the consequences of adverse events.[1]
Individuals may also experience trauma even if the event didn’t happen to them (witnessing a vehicle accident). A traumatic experience can be a single event, a series of events, or adverse childhood experiences (ACEs) that occur over years. Review information about ACEs in Chapter 15.2. There has been an increased focus on the ways in which trauma, psychological distress, quality of life, health, mental illness, and substance misuse are linked. For example, the terrorist attacks of September 11, 2001, the wars in Iraq and Afghanistan, disastrous hurricanes, and the COVID pandemic have moved traumatic experiences to the forefront of national consciousness. Trauma can affect individuals, families, groups, communities, specific cultures, and generations. It can overwhelm an individual’s ability to cope; stimulate the “fight, flight, or freeze” stress reaction; and produce a sense of fear, vulnerability, and helplessness.[2] For more information on stress and coping return to Chapter 2.2 .
For some people, reactions to a traumatic event are temporary, whereas other people have prolonged reactions to trauma with enduring mental health consequences, such as post-traumatic stress disorder, anxiety disorder, substance use disorder, mood disorder, or psychotic disorder. Others may exhibit physical symptoms referred to as somatization, in which psychological stress is expressed through physical concerns such as chronic headaches, pain, and stomachaches. Traumatic experiences can significantly impact how an individual functions in daily life and how they seek medical care.[3]
It is important for nurses to understand that individuals who have experienced trauma are present in all healthcare settings. As noted above, trauma responses can be induced by numerous life events and the effects are correlated with a wide range of medical problems. Individuals may not recognize the significant effects of trauma or may avoid the topic altogether, yet they exhibit emotional responses to their situations that may indicate a trauma history. Likewise, nurses may not ask questions that elicit a patient’s history of trauma. They may feel unprepared to address trauma-related issues proactively or struggle to effectively address traumatic experiences within the constraints of their agency’s policies.[4]
By recognizing that traumatic experiences are closely tied to mental and physical health, nurses can provide trauma-informed care and promote resilience. Trauma-informed care (TIC) is a strengths-based framework that acknowledges the prevalence and impact of traumatic experiences in clinical practice. TIC emphasizes physical, psychological, and emotional safety for both survivors and health professionals and creates opportunities for survivors to rebuild a sense of control and empowerment (i.e., resilience).[5] TIC acknowledges that clients can be retraumatized by unexamined healthcare and community policies and practices and stresses. Acknowledgement that traumatic events may be part of the patient’s current presentation is of utmost importance. Patient-centered care that incorporates the assessment and recognition of trauma rather than applying treatment approaches that do not recognize trauma histories leads to improved patient outcomes.[6]
TIC enhances therapeutic communication between the patient and the nurse. It decreases risks associated with misunderstanding patients’ reactions or underestimating the need for referrals for trauma-specific treatment. TIC encourages patient-centered care by involving the patient in setting goals and planning care that optimizes therapeutic outcomes and minimizes adverse effects. Patients are more likely to feel empowered, invested, and satisfied when they receive TIC.[7]
Implementing a complete program of TIC requires specific training, but it begins with the first contact a person has with an agency. It requires all staff members (e.g., receptionists, direct patient-care staff, nurses, supervisors, and administrators) to recognize that an individual’s traumatic experiences can greatly influence their receptivity and engagement with health services. It can affect their interactions with staff, as well as their responsiveness to care plans and interventions.[8]
View the following YouTube video on trauma-informed approach to health care[9]: Dr. Pickens Explains Trauma-Informed Approach.
It is natural to feel afraid during and after a traumatic situation. The “fight, flight or freeze” reaction caused by the physiological stress response is intended to protect a person from harm. The sympathetic nervous system (SNS) automatically and unconsciously triggers this physiological stress response whenever there is a perception of threat.[10]
- Review the physiology of the sympathetic nervous system and the parasympathetic nervous system in Chapter 6.2.
- Review activation of the stress response in Chapter 2.2.
The SNS activates many organs during the stress response, resulting in symptoms like increased heart rate, increased blood pressure, rapid breathing, and tense muscles. Cumulative adverse childhood experiences can maintain this threat response in people’s brains, which, over time, can “rewire” their level of physiological reactivity to stress and affect emotional regulation like depression, anxiety, and substance abuse. Trauma survivors are also susceptible to chronic physical and mental illnesses and suicide.[11] There also tends to be a decrease in positive social behaviors (such as collaboration and kindness) in individuals experiencing a chronic stress response because it requires their full cognitive capacity to respond by “fighting, fleeing, or freezing.”
Arousal and reactivity symptoms may include the following[12]:
- Being easily startled
- Feeling tense or “on edge”
- Having difficulty sleeping
- Having angry outbursts
These symptoms can make the person feel stressed and angry and can make it hard to do daily tasks, such as sleeping, eating, or concentrating.[13]
Individuals who have a history of trauma may become triggered by engagement with the health care system. They may experience arousal and reactivity symptoms. As a result of the stimulation of the “fight, flight, or freeze” stress response, the parts of the brain involved in memory, planning, decision-making, and regulation may not be engaged. This can impact the patient’s involvement with health care services and affect their ability to adhere to treatment plans.[14] Nurses must understand this potential impact of previous trauma and incorporate patient-centered TIC.
TIC is an approach that uses a lens of trauma to understand the range of cognitive, emotional, physical, and behavioral symptoms potentially seen when individuals enter health care systems. TIC basic goals are to avoid re-traumatization; emphasize survivor strengths and resilience; aid empowerment, healing, and recovery; and promote the development of survivorship skills.[15]
Two influential studies set the stage for the development of TIC[16]:
- The Adverse Childhood Experiences Study was an extensive study involving more than 17,000 individuals from the United States. It analyzed the long-term effects of childhood and adolescent traumatic experiences on adult health risks, mental health, health care costs, and life expectancy.[17]
- The Women, Co-Occurring Disorders, and Violence Study was a study focused on the role of interpersonal and other traumatic stressors among women. The researchers examined the interrelatedness of trauma, violence, and co-occurring substance use and mental health disorders and the incorporation of trauma-informed services.[18]
The Substance Abuse and Mental Health Services Administration (SAMHSA) has defined six core principles of TIC. See Figure 2.3a[19] for an infographic related to these principles[20]:
- Safety: Throughout the organization, patients and staff feel physically and psychologically safe.
- Trustworthiness and transparency: Decisions are made with transparency and with the goal of building and maintaining trust.
- Peer support: Individuals with shared experiences are integrated into the organization and viewed as integral to service delivery.
- Collaboration and mutuality: Power differences between staff and clients and among organizational staff are leveled to support shared decision-making.
- Empowerment voice and choice: Patient and staff strengths are recognized, built on, and validated, including a belief in resilience and the ability to heal from trauma.
- Cultural, historical, and gender Issues: Biases and stereotypes (e.g., based on race, ethnicity, sexual orientation, age, geography) and historical trauma are recognized and addressed.

Trauma-Informed Nursing Practice
Nurses can incorporate trauma-informed care by routinely implementing the following practices with all patients[21]:
- Introduce yourself and your role in every patient interaction: Patients may recognize you, but they may not remember your role. This may lead to confusion and misunderstanding. When a patient understands who you are and your role in their care, they may feel supported in their ability to be actively engaged in their own care. Knowing someone’s name and role can help with building connection and rapport and humanizing the interaction. When one party is nameless, there can be an automatic increase in the power differential between the nurse and patient in the interaction.
- Use open and nonthreatening body positioning: Be aware of your body position when working with patients. Open body language conveys trust and a sense of value. Trauma survivors often feel powerless and trapped. Health care situations can trigger past experiences of lack of control or an inability to escape. Using nonthreatening body positioning helps prevent the threat detection areas of the patient’s brain from taking over and helps patients stay regulated. A trauma-informed approach to body position includes attempting to have your body on the same level as the patient, often sitting at or below the patient. It could also include raising a hospital bed in order for the nurse and the patient to be on the same level, reducing the likelihood of creating a perceived power differential through positioning. Additionally, it is important to think about where you and the patient are positioned in the room in relation to the door or exit. Both nurse and patient should have access to the exit so that neither feels trapped. When in hallways, do not follow traumatized individuals too closely; let them know verbally that you are behind them and on your way elsewhere.
- Provide anticipatory guidance: Verbalize what the patient can expect during a visit or procedure or what paperwork will cover. Past trauma is often associated with unexpected and unpredictable events. Knowing what to expect can reassure patients even if it is something that may cause discomfort. Knowing what to expect reduces the opportunity for surprises and activation of the SNS symptoms. It also helps patients feel more empowered in the care planning process.
- Ask before touching: For many trauma survivors, inappropriate or unpleasant touch was part of a traumatic experience. Touch, even when appropriate and necessary for providing care, can trigger a “fight, flight, or freeze” response and bring up difficult feelings or memories. This may lead to the individual experiencing increased anxiety and activation of the stress response, resulting in disruptive behaviors and possible dissociation. Dissociation is a break in how a person’s mind handles information, causing disconnection from their thoughts, feelings, memories, and surroundings. Nurses are often required to touch patients, and sometimes this touch occurs in sensitive areas. Many nurses instinctively hug patients, especially children. Any touch can be interpreted as unwanted or threatening, so it is important to ask all patients permission to touch them. This includes nursing actions such as obtaining vital signs. Be alert to nonverbal signs such as eye tearing, flinching, shrinking away, or other body language indicating the person is feeling uncomfortable. If the client exhibits signs of discomfort when being touched, additional nursing assessment and perhaps interventions can be implemented such as a mindfulness or grounding practice. Asking permission before you touch patients gives them a choice and empowers them to have control over their body and physical space.
- Protect patient privacy: Family members and other members of the medical team may be present when you care for a patient. Patients may not feel empowered or safe in asking others to step out. It is crucial that nurses do not put the responsibility on the patient to ask others to leave. It is the nurse’s role to ask the patient (in private) whom they would like to be present during care and ask others to leave the room.
- Provide clear and consistent messaging about services and roles: Trust is built when patients experience care providers who are forthright and honest. Dependability, reliability, and consistency are important when working with trauma survivors because previous trauma was often unexpected or unpredictable. Providing consistency from the nursing team regarding expectations and/or hospital rules can help patients feel secure and decrease opportunities for unmet expectations that might lead to triggering disruptive behavior.
- Use plain language and teach-back: Avoid medical jargon and use clear, simple language. When patients are feeling triggered (i.e., their “fight, flight, or freeze” system is engaged), information processing and learning parts of the brain do not function optimally, and it is hard to remember new information. When providing education, information, or instructions, break information into small chunks and check for understanding. Offer to write important details down so they can accurately recall the information at a later time. Use clear language and “teach back” methods that empower patients with knowledge and understanding about their care.
- Practice universal precaution: Universal precaution means providing TIC to all patients regardless of a trauma history. Although ACE screening may be part of routine care, it can also have potential negative effects on patients. Unless a trauma-focused intervention is needed to amend the impact of trauma, many TIC experts propose universal precaution rather than direct screening.
Read a continuing education article titled “Trauma-Informed Nursing Practice” in the American Journal of Nursing.[22]
The Resilient Zone and Self-Regulation Skills
Individuals who have experienced repetitive or cumulative trauma may develop a dysregulated rhythm of their SNS and parasympathetic nervous system (PNS), leaving them reactive and stuck in a state of hyperarousal, hypoarousal, or oscillating between the two extremes as their nervous system attempts to find balance. Simply put, the SNS “activates” the stress response, and the PNS “calms” the stress response. When out of balance, individuals may exhibit behaviors such as substance use disorders, self-harming, violence, poor school and work performance, bullying, and social disengagement.[23] Nurses can enhance patients’ self-regulation skills by encouraging them to pay attention to their “fight, flight, or freeze” symptoms and then sharing skills to balance their SNS and PNS systems.
Self-regulation skills teach patients how to return to a healthy balance of SNS and PNS stimulation called the resilient zone. See Figure 2.3b[24] for an illustration of the resilient zone when the SNS and PNS are in balance. When in the resilient zone, the hormones released by the SNS during the “fight, flight, or freeze” stress response do not block conscious information processing by the brain. This balance promotes better capacity for flexibility and adaptability, prosocial behavior, improved problem-solving, and strategic thinking.[25]
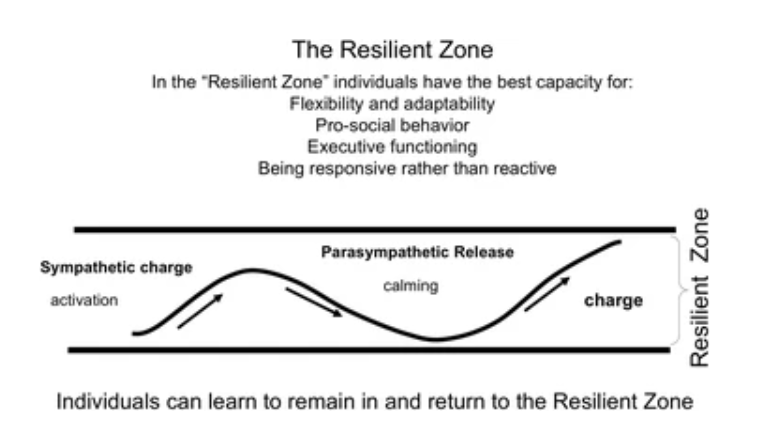
Teaching self-regulation skills enables the individual to pay attention to symptoms of the stress response and use techniques to purposefully stimulate the PNS. They focus on quality of breath, heart rate, and muscle tension and then use relaxation breathing, progressive muscle relaxation, meditation, or other methods to stimulate the PNS. These skills can be used prior to and during challenging events, as well as practiced over time to build deeper nervous system balance.[26]
Resources for self-regulation skills:
App for wellness skills: iChill App — Trauma Resource Institute
- Center for Substance Abuse Treatment (US). (2014). Trauma-informed care in behavioral health services. https://www.ncbi.nlm.nih.gov/books/NBK207201/ ↵
- Center for Substance Abuse Treatment (US). (2014). Trauma-informed care in behavioral health services. https://www.ncbi.nlm.nih.gov/books/NBK207201/ ↵
- Center for Substance Abuse Treatment (US). (2014). Trauma-informed care in behavioral health services. https://www.ncbi.nlm.nih.gov/books/NBK207201/ ↵
- Center for Substance Abuse Treatment (US). (2014). Trauma-informed care in behavioral health services. https://www.ncbi.nlm.nih.gov/books/NBK207201/ ↵
- Center for Substance Abuse Treatment (US). (2014). Trauma-informed care in behavioral health services. https://www.ncbi.nlm.nih.gov/books/NBK207201/ ↵
- Center for Substance Abuse Treatment (US). (2014). Trauma-informed care in behavioral health services. https://www.ncbi.nlm.nih.gov/books/NBK207201/ ↵
- Center for Substance Abuse Treatment (US). (2014). Trauma-informed care in behavioral health services. https://www.ncbi.nlm.nih.gov/books/NBK207201/ ↵
- Center for Substance Abuse Treatment (US). (2014). Trauma-informed care in behavioral health services. https://www.ncbi.nlm.nih.gov/books/NBK207201/ ↵
- Washington State Health Care Authority. (2019, June 24). Dr. Pickens explains trauma-informed approach [Video]. YouTube. All rights reserved. https://youtu.be/6syEFO4OSFU ↵
- This work is a derivative of Action steps using ACEs and trauma-informed care: A resilience model by Laurie Leitch and is licensed under CC BY 4.0 ↵
- Trauma-Informed Care Implementation Resource Center. (n.d.). What is trauma-informed care? Center for Health Care Strategies. https://www.traumainformedcare.chcs.org/what-is-trauma-informed-care/ ↵
- National Institute of Mental Health. (2019, May). Post-traumatic stress disorder. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd ↵
- National Institute of Mental Health. (2019, May). Post-traumatic stress disorder. U.S. Department of Health and Human Services. https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd ↵
- Fleishman, J., Kamsky, H., & Sundborg, S. (2019, May 31). Trauma-informed nursing practice. OJIN: The Online Journal of Issues in Nursing, 24(2). https://doi.org/10.3912/OJIN.Vol24No02Man03 ↵
- Tracy, E. E., & Macias-Konstantopoulos, W. (2021, August 19). Human trafficking: Identification and evaluation in the health care setting. UpToDate. Retrieved April 4, 2022, from www.uptodate.com ↵
- Center for Substance Abuse Treatment (US). (2014). Trauma-informed care in behavioral health services. https://www.ncbi.nlm.nih.gov/books/NBK207201/ ↵
- Felitti, V. J., Anda, R. F., Nordenberg, D., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experience (ACE) study. American Journal of Preventive Medicine, 14(3), 245-258. https://doi.org/10.1016/S0749-3797(98)00017-8 ↵
- Clark, H. W., & Power, A. K. (2005). Women, co-occurring disorders, and violence study: A case for trauma-informed care. Journal of Substance Abuse Treatment, 28(2), 145-146. https://doi.org/10.1016/j.jsat.2005.01.002 ↵
- Centers for Disease Control and Prevention and in the Public Domain. Access for free at https://stacks.cdc.gov/view/cdc/138924/cdc_138924_DS1.pdf ↵
- Trauma-Informed Care Implementation Resource Center. (n.d.). What is trauma-informed care? Center for Health Care Strategies. https://www.traumainformedcare.chcs.org/what-is-trauma-informed-care/ ↵
- Fleishman, J., Kamsky, H., & Sundborg, S. (2019, May 31). Trauma-informed nursing practice. OJIN: The Online Journal of Issues in Nursing, 24(2). https://doi.org/10.3912/OJIN.Vol24No02Man03 ↵
- Dowdell, E., & Speck, P.M. (2022). Trauma-informed care in nursing practice. American Journal of Nursing, 122(4), 30-38. https://journals.lww.com/ajnonline/Fulltext/2022/04000/CE__Trauma_Informed_Care_in_Nursing_Practice.22.aspx ↵
- This work is a derivative of Action steps using ACEs and trauma-informed care: A resilience model by Laurie Leitch and is licensed under CC BY 4.0 ↵
- Leitch, L. (2017). Action steps using ACEs and trauma-informed care: A resilience model. Health Justice 5, 5. https://doi.org/10.1186/s40352-017-0050-5 ↵
- This work is a derivative of Action steps using ACEs and trauma-informed care: A resilience model by Laurie Leitch and is licensed under CC BY 4.0 ↵
- This work is a derivative of Action steps using ACEs and trauma-informed care: A resilience model by Laurie Leitch and is licensed under CC BY 4.0 ↵
An event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful and can have lasting adverse effects on the individual’s functioning and physical, social, emotional, or spiritual well-being.
The ability to rise above circumstances or meet challenges with fortitude.
Traumatic circumstances experienced during childhood such as abuse, neglect, or growing up in a household with violence, mental illness, substance use, incarceration, or divorce.
Psychological stress is expressed through physical concerns such as headaches and stomachaches.
A strengths-based approach to providing client care that is grounded in an understanding of the impact of trauma. It emphasizes physical, psychological, and emotional safety for both providers and survivors and creates opportunities for survivors to rebuild a sense of control and empowerment referred to as resilience.
Part of the autonomic nervous system that activates the 'fight or flight' responses such as increases in heart rate and respiratory rate.
A break in how a person’s mind handles information, causing disconnection from their thoughts, feelings, memories, and surroundings.
Healthy balance of SNS and PNS stimulation.

